Researchers from Korea and Japan shared the results of innovative approaches to pancreatic beta-cell regeneration in diabetic patients at the 34th Spring Conference hosted by the Korean Diabetes Association on Saturday.
Two experts from each country -- Professors Kim Hyeong-seok of Chungnam National University College of Medicine, Lee Myung-shik of Yonsei University College of Medicine, Shinsuke Tokumoto of Kyoto University, and Masayuki Shimoda of Japan's National Center for Global Health and Medicine -- presented potential therapeutic options associated with pancreatic issues for diabetes patients.
Professor Kim explained how lactation improves pancreatic beta-cell mass and function through serotonin production. His study results suggested that serotonin mediates the long-term beneficial effects of lactation on women's metabolic health with increased beta-cell proliferation and lowered oxidative stress.
Professor Kim’s research team confirmed the long-term beneficial effects of lactation on beta-cell function, which lasts for years.
Kim noted that pregnancy imposes a substantial metabolic burden on women with weight gain and insulin resistance. During lactation, prolactin-induced serotonin production in beta cells and the serotonin stimulated beta-cell proliferation. In addition, intracellular serotonin acted as an antioxidant to mitigate oxidative stress and improved beta-cell survival.
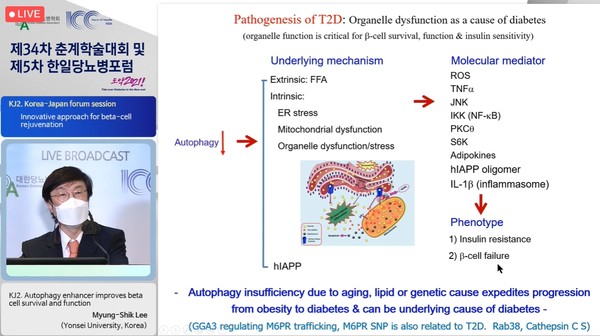
Professor Lee said that autophagy enhancers could potentially help patients fight against diabetes characterized by islet amyloid accumulation.
According to Lee, a recently identified autophagy enhancer (MSL-7) reduced simian IAPP (sIAPP) and hIAPP oligomer accumulation, improving glucose profile and fatty liver of obese mice with increased lipolysis while lowering metabolic inflammation.
Lee said he found that 90 percent of diabetic patients had islet amyloid deposition due to differences in the amino acid sequences of islet amyloid polypeptide (IAPP). Islet, a part of the pancreas, contains several types of cells, including beta cells that produce insulin to break down food and regulate glucose.
"We have reported that autophagy plays a key role in clearing amyloidogenic human IAPP (hIAPP) oligomer," Lee said. "We found potential management by using autophagy enhancer, which could work as a therapeutic modality against diabetes characterized by islet amyloid accumulation."
Professor Tokumoto presented a new animal model for beta-cell proliferation assessment, which could relieve the diabetes progression.
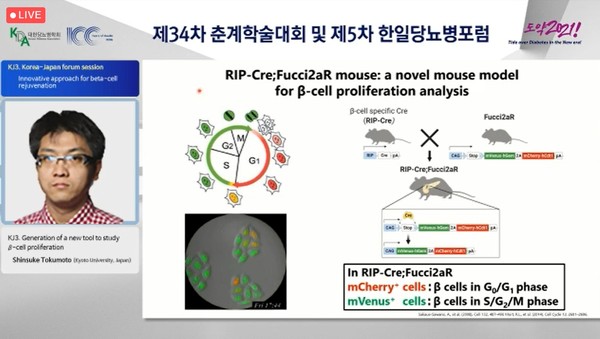
Tokumoto explained that various factors potentially affect beta-cell replication. Still, the current knowledge is limited due to unstandardized assay and lack of alternative methods. In his study, researchers tried to generate a novel mouse model that could help find a more accurate quantification of beta-cell proliferation using a cell cycle monitoring biosensor (Fucci2a).
"We have found a strong link between the islet size and the amount of beta-cell, which suggests that the novel mouse model could be used as a new tool for beta-cell proliferation assessment," Tokumoto said.
Professor Shimoda said that Japan has recently confirmed positive results from the phase 3 clinical trials of the Clinical Islet Transplantation Study (CIT)-07 protocol. The study's primary endpoint was to prevent severe hypoglycemia while maintaining HbA1c below seven percent.
Shimoda explained that islet transplantation could be a promising treatment to reduce hypoglycemia and provide excellent glycemic control.
"The Edmonton Protocol reported by the University of Alberta in 2000 showed that islet transplantation is a promising treatment for type 1 diabetes," he said, adding that Japan has approved and granted public health insurance for the transplant. The method became a standard therapy in 2020.
However, he pointed out, the shortage of donors poses a limitation to providing islet transplantation for more patients in need of surgery. To overcome this problem, many ways to secure cell sources have been explored by researchers in Japan.
"Once the donor shortage problem can be solved, islet transplantation for insulin independence in type 2 diabetes patients with reduced insulin secretion, which is more prevalent in Asians, can be considered as the next target," Shimoda said. "The next-generation islet transplantation therapies are expected to be developed with further studies."

