“Unlike other cancers, hepatocellular carcinoma (HCC) is mostly diagnosed non-invasively. But this has not been reflected in the health policy and there is an unmet need in this area. Expansion of reimbursement for HCC treatments is also slow. I hope the government could reflect clinical situations to ease reimbursement criteria and allow the use of drugs recommended by international guidelines for patients in urgent need.”
So said professor Jang Eun-sun of the Internal Medicine Department at the Seoul National University Hospital, speaking on the need for reimbursement for HCC at The Liver Week 2021, a virtual conference of the Korean Association for the Study of the Liver (KASL) on Thursday.
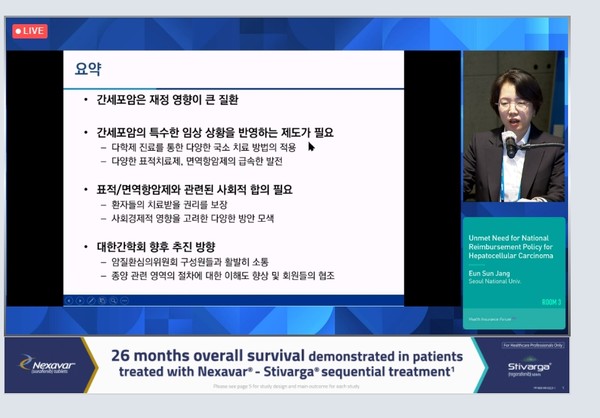
Jang is the insurance committee director at KASL and leader of the insurance committee at the Korean Liver Cancer Association (KLCA).
According to Jang, liver cancer causes the largest financial burden for patients, and it is costlier than lung cancer and gastric cancer.
Patients with the chronic liver disease face cost increase according to the disease progression. Chronic hepatitis costs about 1 million won ($885) annually, liver cirrhosis, 2 million won, and liver cancer, 8 million won. Jang said economic burdens from liver cancer are so large that they could affect the nation’s finance.
She noted that physicians use non-invasive diagnostic methods to detect HCC because it mostly occurs in patients with underlying liver disease, and HCC poses a high risk of bleeding in a biopsy.
Also, HCC’s hypervascularity makes imaging diagnosis highly accurate, she added.
In the process of the government’s reimbursement expansion for abdominal MRI, the government relaxed criteria to make non-invasive diagnosis easier for patients with suspected HCC. As a result, if a dysplastic nodule is found in the liver, an MRI can be covered by health insurance once a year.
Still, several issues have not been addressed in HCC treatment, Jang said.
“When we take PET-CT, insurance benefits for other solid cancers are recognized in the case of diagnosis, determination of effects during treatment, and stage re-establishment, but those for HCC are limited,” she said. “Reimbursement is allowed only for patients who plan to undergo liver transplantation or resection. In recurrence decision, only those with suspected recurrence get insurance benefits.”
Jang emphasized that reimbursement for HCC treatment was urgent.
Anticancer drugs do not work well on HCC. Most patients who can receive anticancer therapy have a poor liver function, which has made it difficult for pharmaceutical firms to develop a treatment for HCC, she explained.
However, several latest drugs produced successful clinical outcomes, and guidelines by the European Society for Medical Oncology (ESMO) and the U.S. National Comprehensive Cancer Network (NCCN) have changed accordingly, she added.
In Korea, only Nexavar (sorafenib) and Lenvima (lenvatinib) in the first-line treatment and Stivarga regorafenib in the second-line treatment is reimbursable. Nexavar got the insurance benefits in 2007, but the reimbursement has not been broadened for over a decade.
First-line therapy Tecentriq (atezolizumab)+Avastin (bevacizumab) and second-line treatments Cabometyx (cabozantinib) and Cyramza (ramucirumab) are all recommended highly in other countries. However, local patients have to pay 100 percent out of pocket to receive those treatments.
“Reimbursement for many HCC treatments have been frequently rejected,” Jang said.
KASL was doing its best to make Tecentriq+Avastin reimbursable first, she went on to say.
“The combo treatment should be reimbursable because its study design included data to evaluate the quality of life,” Jang said. “So, it is possible to estimate the incremental cost-effectiveness ratio (ICER), considered the most important in calculating the fiscal impact.”
Although Cabometyx demonstrated excellent survival data and accumulated three-year treatment experience after winning approval in 2017, its fiscal impact has yet to be reviewed, and discussion remains incomplete, Jang added.
“Targeted therapies and immunotherapies provide very limited treatment options and require astronomical treatment costs,” she said. “This affects the government’s finance, too. So, we need sufficient social consensus (on allowing reimbursement for those therapies).”

