A research team at the Seoul National University Bundang Hospital (SNUBH) has released the results of phase 1 clinical trial of a new treatment that kills cancer cells of pancreatic cancer patients. In the trial, the researchers tested a method that used “genetically modified adenovirus,” in which two different cancer treatment genes are inserted, on patients with irresectable pancreatic cancer.
Pancreatic cancer is deadly cancer that people fear most because of its poor prognosis, as shown by a five-year survival rate of only about 12.2 percent.
Patients with locally advanced pancreatic cancer, in which cancer cells spread to nearby lymph nodes and blood vessels, face difficulty in receiving surgery and growing resistance to anticancer treatment, resulting in the abandonment of therapy. With the recent rapid development of cancer treatments, however, anticancer therapies based on precision medicine get the spotlight, and new therapies are being studied for pancreatic cancer.
These new therapies are drawing attention as to whether they provide hope for patients with pancreatic cancer whose vein or artery.
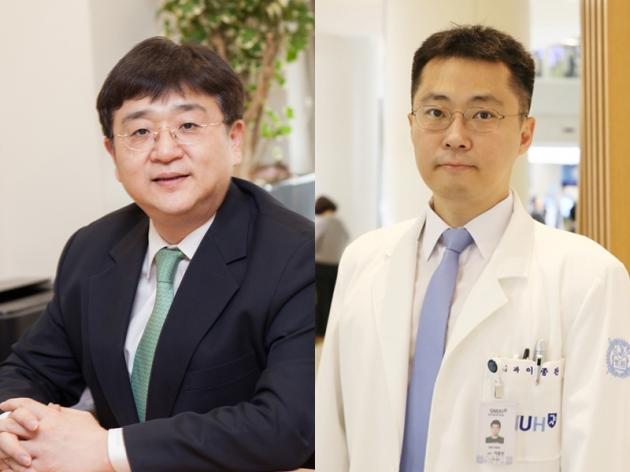
The research team, led by Professors Hwang Jin-hyuk and Lee Jong-chan, studied to confirm the safety and possibility of a new way to treat non-resectable pancreatic cancer patients with adenovirus as a gene carrier in nine patients for two years from August 2018.
The team inserted an adenovirus that can create two enzymes -- cytosine deaminase and tyrosine kinase -- to pancreatic cancer patients through endoscopic ultrasonography. The injected adenovirus naturally disappears in healthy cells and multiplies only in pancreatic cancer cells due to the primary effect of genetic modification.
After the injection, if the patient takes an oral medication without an anticancer effect, the drug meets the enzyme of the adenovirus in the pancreatic cancer cell and turns into an anticancer reagent. The changed virus, which can survive in cancer cells, then kills only pancreatic cancer cells.
The study result showed that drug administration to the nine pancreatic cancer patients did not show significant side effects during 12 weeks of treatment, proving to be a relatively safe medicine. Pancreatic cancer did not progress further in all nine patients who have been taking 12 weeks of treatment. The median progression-free survival, which is used as an index for evaluating the efficacy, was 11.4 months.
“The study was meaningful as we could confirm the safety and potential of new gene therapy via the phase 1 trial,” Professor Hwang said. “We not only confirmed that the patients could be treated by inserting the modified genes to pancreatic cancer but also saw the effect of slowing the progression of pancreatic cancer, providing a basis for follow-up studies.”
The trial results were published in the latest issue of Gastrointestinal Endoscopy, a U.S. journal with top authority in the endoscopic field.

