
Local researchers said they have proved the safety and efficacy of proton beam radiotherapy (PBT) in patients with hepatocellular carcinoma (HCC) for the first time in the world.
The U.S., Europe, and Japan have applied PBT to HCC patients earlier, but Korea confirmed its efficacy and safety ahead of them, they said.
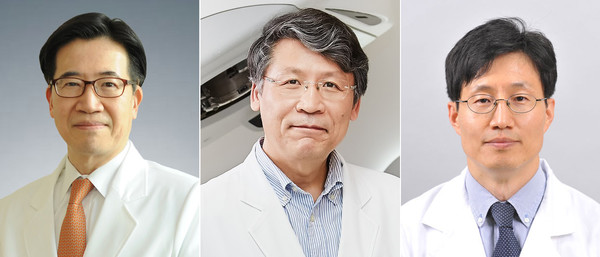
The research trio at National Cancer Center -- Professors Park Joong-won of the Center for Liver and Pancreatobiliary Cancer, Kim Tae-hyun of the Center for Proton Therapy, and Koh Young-hwan of the Department of Radiology -- said they have identified the effect of PBT in a prospective, randomized, controlled, investigator-initiated, and phase-3 study.
The team has conducted the study since 2013. The state cancer center introduced PBT in Korea in 2007. They have published the results of the research in the Journal of Hepatology recently.
PBT has been used for HCC patients worldwide, but there were no randomized, controlled trials that compared PBT outcomes and standard care, such as radiofrequency ablation (RFA). Physicians recommend resection or RFA for HCC smaller than three centimeters.
The research team randomly assigned 144 HCC patients to 72 PBT group and 72 RFA group. However, the team allowed the treatment switch, and 80 went to the PBT group and 56, the RFA group.
The results showed that the two-year local progression-free survival (LPFS) rate was 94.8 percent in the PBT arm, versus 83.9 percent in RFA. The three- and four-year LPFS rates for PBT were also non-inferior to those for RFA.
Patients treated with PBT because RFA was impossible outnumbered those in opposite cases.
Among the 72 patients initially assigned to the RFA group, 22 (30 percent) could not receive RFA, and 19 crossed over to the PBT group. In contrast, 11 out of the 72, or 15 percent, in the PBT group could not receive PBT, and six of them received RFA instead.
Among common adverse effects were radiation pneumonitis (32.5 percent) and decreased leukocyte counts (23.8 percent) in the PBT group. In comparison, increased alanine aminotransferase levels (96.4 percent) and abdominal pain (30.4 percent) were relatively common in the RFA group. There were no serious adverse effects or morality in both of the groups.
PBT for HCC usually requires 10 times of 30-minute session per day for about two weeks and is covered by the national health insurance.
Park, the corresponding author, said PBT is a state-of-the-art technology expanding the scope of liver cancer treatment.
“This study overcame various limitations of phase-3 research by using a non-inferiority method and finally proved that PBT could cure recurrent HCC,” he said.
First author Kim, who is head of the NCC’s Center for Proton Therapy, said PBT is a non-invasive treatment causing no bleeding and no pain by accurately targeting only cancer cells.
“As a new treatment that can complement the weaknesses of the existing standard care RFA, I hope it will help more HCC patients,” he said.

