Lung cancer patients who have smoked long and with relatively fewer cases of metastasis to the brain showed stronger resistance to targeted therapies, Severance Hospital said Friday based on patient research.
A research team, led by Professors Ahn Beung-chul, Lee Ji-hyun, and Hong Min-hee of Lung Cancer Center at Yonsei Cancer Hospital, has found two characteristics of patients resistant to EGFR (Epidermal Growth Factor Receptor)-Tyrosine Kinase Inhibitor (TKI) therapy in non-small cell lung cancer (NSCLC) caused by EGFR mutation -- long-term smoking and fewer brain metastases.
NSCLC accounts for 80-85 percent of total lungs cancer. Various mutations like EGFR, Anaplastic Lymphoma Kinase (ALK), and Reactive Oxygen Species (ROS1) can cause NSCLC. Of these, EGFR takes up 30-40 percent of NSCLCs.
Tyrosine Kinase Inhibitor (TKI) treatment that targets EGFR mutants consists of Gefitinib and Erlotinib as the first-generation TKI, and Afatinib and Dacomitinib as the second-generation TKI. However, using these drugs for 10 to 12 months leads to the rejection of the treatment. Hence, the third-generation TKIs, including Osimertinib, are applied. And, between 5 and 22 percent of the resistance to first to third-generation TKIs is caused by MET mutation.
The team analyzed 186 patients at Yonsei Cancer Hospital who had failed first to third-generation EGFR-TKI treatment from 2004 to 2019. Of them, the team compared patients who showed positive MET amplification to negative ones. Thirty 30 patients, or 16.1 percent, showed positive MET-amplification.
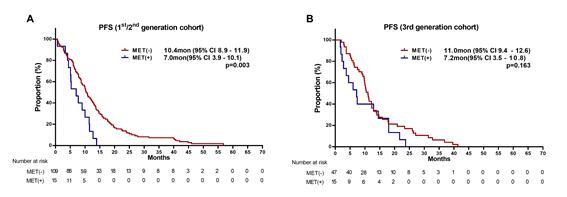
The progression-free survival (PFS) period, where aggravation is on halt, showed a difference between first and second-generation TKI patients. The median PFS of MET-amplification positive patients was seven months, shorter than the 10.4 months of negative patients. Compared with the third-generation patients, no noticeable difference was found.
The factors that led to the cause of MET amplification were smoking and brain metastases. In the case of smokers, the rate of MET-amplification was 3.5 times higher than that of non-smokers. Also, patients with no brain metastases had 86 percent lower chances of MET-amplification than that of patients that had the spread of cancer to the brain.
The research has helped establish criteria for selecting patients who need MET-amplification positive test, including smokers and those with fewer brain metastases, and set a new guideline to decide whether they have MET-amplification tests or not, the hospital said.
Drug tolerant patients who smoke and have fewer brain metastases may go through the test and proceed with the following treatments, it added.
“Smoking and fewer brain metastases increase the chances of MET-amplification and resistance to EGFR-TKI therapy,” Professor Lee said. “The research results will help the research and development of MET-mutant targeted therapy.”


