The 2021 International Congress of Diabetes and Metabolism (ICDM) kicked off its three-day online conference on Thursday. Sponsored by the Korean Diabetes Association (KDA), ICDM celebrates its 11th anniversary of discussing diabetes and endocrine systems.
Notably, the conference put a lot of its focus on how the Covid-19 pandemic has affected diabetes patients this year.
In a session titled “Diabetes and Covid-19,” diabetes experts from Korea, Hong Kong, Japan, and Taiwan talked about the effects of the Covid-19 pandemic on diabetes patients.
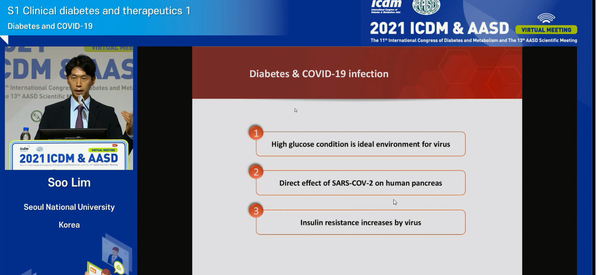
In the first session, Professor Lim Soo of the Seoul National University Hospital presented how Covid-19 affects diabetes from a pathophysiological perspective to clinical management. According to Lim, glucose, and glutamine is a good energy source for viruses.
“When blood glucose level is high, it sets a good environment for the virus to grow. Therefore, in the current Covid-19 pandemic, diabetes patients must have good control over their glucose level,” Lim said. “The Covid-19 virus could adversely affect a person’s endocrine and exocrine pancreas.”
Professor Lim noted that angiotensin-converting enzyme 2 (ACE2), a gene expressed in the human pancreatic beta cells, and ACE2 could act as an entry gene for Covid-19 into the human body.
“This means that it can directly affect the human body as the Covid-19 virus can be replicated in the human pancreatic islets, resulting in an impartment of pancreatic beta-cell functions,” he said.
The Covid-19 can also induce inflammation, which, in turn, can lead to insulin resistance as it can affect T-cell immunity directly, leading to an increase in interferon-gamma and interleukin 6 (IL-6) secretion.
Lim stressed that interferon-gamma could lead to increased insulin resistance in muscle tissue in people with obesity or pre-diabetes and IL-6 induces dysregulation metabolic homeostasis.
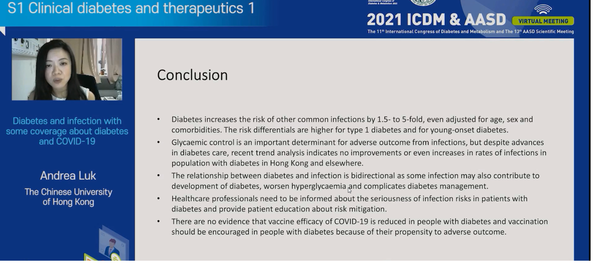
A foreign participant stressed the need for diabetes patients to receive vaccinations.
“While there is no evidence that diabetes increases the risk of acquiring Covid-19, there is ample evidence that diabetes worsens the prognosis,” Professor Andrea Luk at the Chinese University of Hong Kong said. “Regarding Covid-19 vaccinations for diabetes patients, there are currently more questions than answers.”
However, studies have proved that antibody response to multiple antigens of Covid-19 is similar between diabetics and non-diabetics, she added.
Luk noted that as neutralizing antibodies predict survival in people regardless of diabetes, people with diabetes should receive the vaccine as there is no evidence that diabetes reduces the vaccine's efficacy.
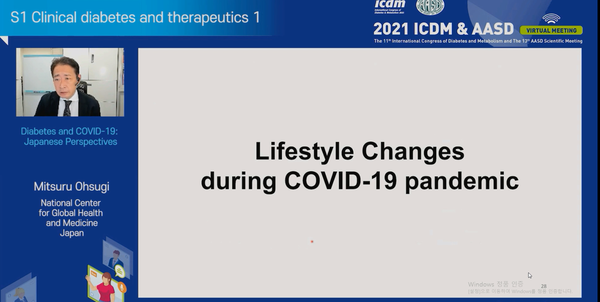
Professor Mitsuru Ohsugi at the National Center for Global Health and Medicine commented on the lifestyle changes and outpatient diabetes care during the Covid-19 era.
“In a study involving 321 patients with diabetes conducted in Japan, we were able to confirm that while there were no significant changes to the hemoglobin A1c (HbA1C), HbA1C level did rise when the patient had less physical activity due to the Covid-19 pandemic,” Ohsugi said. “We also confirmed that HbA1C levels tended to increase as more people started working from home than going to work.”
However, the team confirmed that even during the pandemic, patients with companion animals such as dogs had lower HbA1C levels than those who did not have pets, he added.
Ohsugi stressed that the results show the need to improve inpatient diabetes management and outpatient diabetes care.
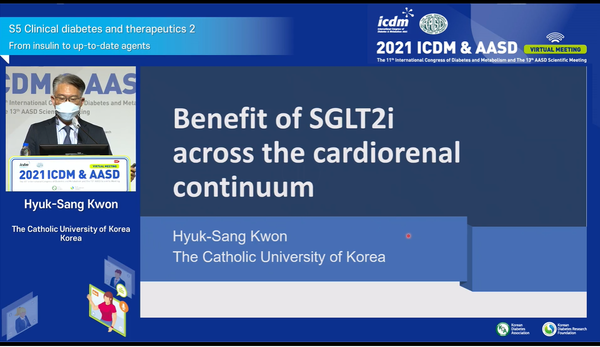
Another Korean expert, Professor Kwon Hyuk-sang of the Catholic University of Korea, explained the benefit of SGLT2 inhibitor (SGLT2i) across the cardiorenal continuum.
As studies suggest, Kwon said that a dual combination of SGLT2i with metformin might be better as first-line therapy for patients. “The benefits of SGLT2i inhibitors across the cardiorenal continuum are true, but we need more robust evidence to wait and see,” he said.
Professor Kwon explained that the cardiovascular and renal systems are closely interconnected in health and disease.
A cardiorenal syndrome is broadly defined as a disorder of the heart and kidney whereby acute or chronic dysfunction in one organ may induce problems in each organ. Thus, the syndrome represents concomitant cardiovascular and chronic kidney disorders (CKD) that result from systemic disease with a common pathway.
Both diseases progress through a continuous chain of events, defined as the cardiorenal continuum initiated by risk factors that lead to subclinical disease, clinical events, and ultimately to heart failure and end-stage kidney disease.
More recently, clinical trials with SGLT-2 inhibitors (SGLT2i) have shown a significant reduction in cardiovascular and kidney outcomes, and the beneficial effects of SGLT2i have been observed across all stages of the cardiorenal continuum ranging from patients with diabetes to multiple risk factors.
Kwon explained that four big clinical trials using four different SGLT2 inhibitors showed significant outcomes in the past.
“SGLT2i showed beneficial effects on heart failure hospitalization renal outcomes in different clinical trials and recovered broader spectrum and stages of cardiorenal continuum,” Kwon said.
The professor added that the recent regulatory guidelines recommend an initial dual combination with metformin and SGLT2 inhibitors for CKD patients with early type 2 diabetes.
Kwon also said, “The recent primary care for diabetes in Europe defined metformin as the first-line therapy in patients with type 2 diabetes and recommended providing a combination of metformin and SGLT2i.”
The same combination of metformin and SGLT2i was also recommended for patients with atherosclerotic cardiovascular disease (ASCVD) as regulators considered patients with type 2 diabetes to be at high risk.
“Type 2 diabetes has been traditionally described as a progress of the disease as one’s blood sugar levels will gradually increase over time, and more medications such as insulin will be needed eventually,” Kwon said. “In the last few decades, the treatment paradigm has shifted and found that proactive management in early-stage diabetes can help prevent progress and complication.”

