Nonsteroidal anti-inflammatory drugs (NSAIDs) largely negated the effect of clodronate, the first-generation bisphosphonate (BP) to treat osteoporosis in adults, and NSAIDs’ interactions with next-generation osteoporosis drugs should be urgently investigated, a study said.
On Wednesday, the Journal of Bone and Mineral Research (JBMR) published a study titled, “Potential Adverse Effect of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) on Bisphosphonate Efficacy: An Exploratory Post Hoc Analysis From a Randomized Controlled Trial of Clodronate.”

NSAIDs are one of the most commonly prescribed drugs for various acute and chronic musculoskeletal or inflammatory diseases.
U.S. statistics showed that 96.4 percent of the seniors aged 65 or more use NSAIDs, and 32.9 percent take NSAIDs regularly for more than one month.
NSAIDs have a weak but beneficial effect on bone health, but many epidemiological studies reported conflicting results, and the issue remains debatable.
In a retrospective analysis, the research team investigated the effect of NSAIDs on fracture risk in patients who used clodronate, the first-generation bone resorption inhibitor BP.
Among 5,212 women recruited to the study, 1,082 (21 percent) used NSAIDs at the study entry. The most commonly reported drugs were ibuprofen and diclofenac.
Users of NSAIDs had a slightly lower average age than non-users (79 vs. 80), weighed more (66.7kg vs. 64.7kg), and had slightly higher bone density in the femoral neck (0.66 g/cm2 vs. 0.64 g/cm2).
The results showed that NSAIDs use during the three-year study was associated with an increase in osteoporotic fracture risk, although the association was not statistically significant.
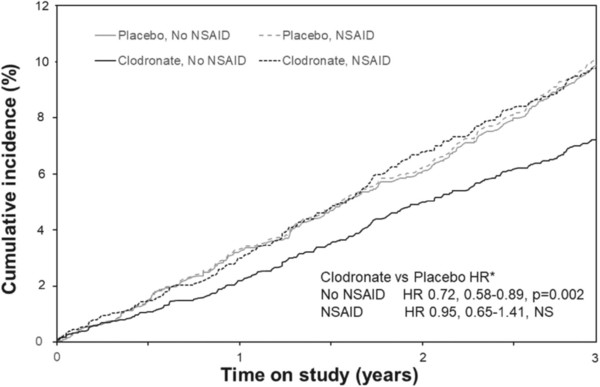
In women receiving clodronate, the effect of the BP to reduce osteoporotic fracture risk was not observed in those receiving NSAIDs, in contrast to the non-users.
In a subset with hip bone mineral density (BMD) repeated at year 3, BMD loss during clodronate therapy was greater in those women receiving NSAIDs than in non-users (total hip -2.75 percent versus -1.27 percent, femoral neck BMD -3.06 percent versus -1.12 percent).
In other words, the efficacy of clodronate to reduce fracture risk was largely negated in those receiving NSAIDs, the research team said.
“The observation that NSAID use significantly reduced the ability of clodronate to prevent bone loss and fractures is unique and of high clinical importance,” the research team said. “Imbalances do not mediate the marked reduction in baseline characteristics or lower compliance efficacy.”
Although researchers need to study further possible mechanisms, it is urgent to examine the interaction in studies of other BPs in osteoporosis and other bone diseases because NSAIDs and BPs are usually combined, the research team said.

