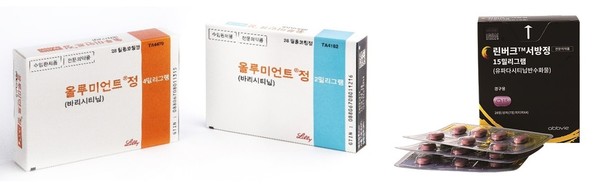
Lilly’s Olumiant (baricitinib) and Abbvie’s Rinvoq (upadacitinib) got health insurance benefits starting from May 1 to treat severe atopic dermatitis.
Patients who used the two drugs to treat severe atopic dermatitis without health insurance will be able to get insurance benefits as long as they meet certain criteria, the government said.
The Health Insurance Review and Assessment Service (HIRA) released Q&As related to the reimbursement criteria for Olumiant and Rinvoq and how to use them continuously for patients who used the two drugs without reimbursement.
Health insurance coverage became available for Olumiant and Rinvoq to treat serious atopic dermatitis on May 1.
The reimbursement was granted to adult patients with chronic severe atopic dermatitis who have been suffering symptoms for three years or longer.
More specifically, patients who could not control the disease after using a local treatment for four weeks or more as the first-line treatment, and those who do not respond to a systemic immunosuppressant for three months or longer or who cannot use such drug due to side effects, and whose EASI score is 23 or higher, can receive the insurance benefits.
HIRA also prepared a support measure for patients who used to receive Olumiant or Rinvoq without reimbursement before May.
“If a patient has been taking Olumiant or Rinvoq before the reimbursement and meets the current criteria at the time of the initial administration of the treatment, HIRA will recognize the insurance benefits,” HIRA said.
Also, patients who are outside the reimbursement criteria but meet the following conditions can enjoy insurance benefits -- a confirmed history of administration of systemic immunosuppressant (cyclosporine or methotrexate) after atopic dermatitis diagnosis, or having records of indicators of the severity of atopic dermatitis before the administration of systemic immunosuppressant (EASI 23 or higher, SCORAD 40 or higher, and IGA score of 4).
Patients meeting the criteria will have the reimbursement recognized for six months. If they maintain the status of the initial benefit after six months, they can receive a continued administration. From the beginning of the reimbursement, doctors must record EASI scores.
These measures will be effective on patients who apply for insurance benefits by Oct. 31 and whose benefits get recognized.
HIRA said it would recognize the indicators of the severity of atopic dermatitides, such as SCORAD and IGA, when evaluating response to systemic immunosuppressants in patients who did not undergo the EAST test before getting systemic immunosuppressant.
If the score does not decrease by 50 percent after administering a systemic immunosuppressant, the patient is considered not responding to the systemic immunosuppressant.
In this case, the patient should undergo an EASI test and score 23 or more before administering Olumiant or Rinvoq to get insurance benefits.
Indicators of severity other than EASI score can be limitedly applied to patients who started Olumiant or Rinvoq administration until Oct. 31.
HIRA noted that if a patient gets Olumiant or Rinvoq immediately after the first-line local treatment without systemic immunosuppressant administration, the patient must pay the full cost of the drug.
“Still, if it is impossible to use systemic immunosuppressant due to medical contraindications such as renal failure, uncontrolled hypertension, uncontrolled infection, malignant tumor, or severe liver disease, benefits will be recognized when the patient meets the EASI score condition,” the agency said.
Suppose a patient briefly stopped the medication before the first response evaluation (at week 16) for medical reasons. In that case, the resumption of the drug will be reimbursable if the initial EASI score was 23 or higher, HIRA went on to say.
If a patient stops the treatment after the initial response evaluation at week 16, the withdrawal period of fewer than three months will be recognized as continuous treatment administration. However, if the period is more than three months, the reimbursement will be recognized when the EASI score is 23 or more at the initial administration, HIRA added.

