Empirical antibiotic therapy, or the use of antibiotics before testing bacterial infection in Covid-19 patients, does not improve Covid-19 patients’ clinical outcomes, a study showed.
Empirical antibiotic therapy is defined as the use of antibiotics within 48 hours after hospitalization before microbiological documentation of bacterial infection.
Korea’s Covid-19 treatment guidelines do not recommend prescribing antibiotics, but some physicians still prescribe antibiotics to Covid-19 patients according to their medical judgment.
A research team at the Seoul National University Hospital released their study that evaluated whether empirical antibiotic therapy was beneficial to improving Covid-19 patients’ clinical results in the Journal of Korean Medical Science (JKMS).
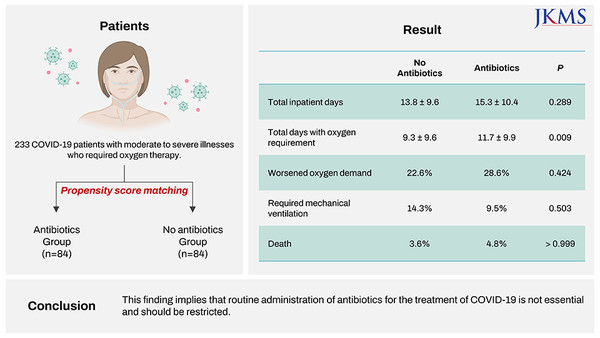
The research team investigated whether 233 patients with moderate to severe Covid-19 who needed oxygen treatment received empirical antibiotic therapy between January 2020 and August 2021. Among the 233 patients, 117 did so, and 116 did not.
Then, the research team selected 84 patients who received empirical antibiotic therapy to match another 84 without antibiotics who had similarities in demographic and clinical characteristics.
The team compared their length of stay, days of oxygen treatment, and incidence of death during isolation.
The results showed that empirical antibiotic therapy did not positively impact Covid-19 patients’ clinical prognosis.
Those with empirical antibiotic therapy stayed isolated for 15.3 days, versus 13.8 days in the group without antibiotics.
The treatment group had 11.7 days of oxygen treatment vs. 9.3 days among those without antibiotics.
The proportion of patients with increased oxygen demand was 28.6 percent in the antibiotic group, vs. 22.6 percent in the group without antibiotics.
The mortality rate during isolation was 4.8 percent among patients with empirical antibiotic therapy, compared with 3.6 percent among those without it. There was little difference in the death rate between the two groups.
“This study showed that empirical antibiotic therapy does not improve clinical outcomes in moderate to severe Covid-19 patients,” the research team said. “Unnecessary use of broad-spectrum antibiotics leads to the emergence of multidrug-resistant organisms.”
The research team concluded that antibiotics should only be prescribed sparingly, based on the best available evidence for Covid-19 patients.
The study was the first to report the relationship between empirical antibiotic therapy and the prognosis of moderate to severe Covid-19 patients.
“These findings support current guidelines that routine administration of antibiotics for treatment of Covid-19 is not essential,” the research team added.

