Five years have passed since Korea introduced the life-prolonging treatment decision system, but it still has too many shortcomings, including the timing to decide its discontinuance, establishing medical institutions’ ethics committees, and educating medical workers.
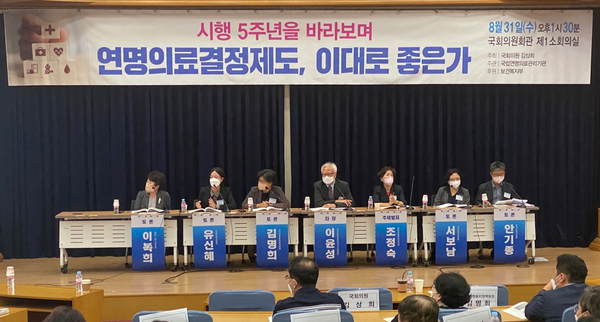
Experts pointed out these and other problems at a symposium, “Can the five-year-old life-prolonging treatment decision system go on like now?” at the National Assembly on Wednesday. Rep. Kim Sang-hee of the opposition Democratic Party of Korea and the National Agency for Management of Life-Sustaining Treatment co-organized the workshop.
Cho Jeong-suk, head of the Life-Sustaining Medical Care Management Center under the National Bioethics Policy Board, made a presentation, “The operation of life-sustaining care decision system and tasks for its improvement.”
According to the board, there are 568 institutions where people can register their advance directives in Korea. Ongjin Country in Gyeonggi Province recently became the last lower-level locality that opened such an office.
From 2018 to 2021, the cumulative number of advance directives totaled 1,158,585.
By age, 15.5 percent of people in their 70s had prepared the advance directives as of June 30, and 11.5 percent of those in their 80s. Among people 65 and older, 11.6 percent had submitted advance directives.
However, Cho pointed out that there is room for improvement concerning their registrations, such as expanding the scope of registration offices to public health centers and senior welfare centers, guaranteeing self-determination rights according to registered advance directives, and strengthening counselors' capacity at registration offices.
The number of medical institutions that have established an ethics committee nearly doubled from 164 in 2018 to 330 in 2022, and that of general hospitals with an ethics committee also doubled from 91 to 180 during the period, according to Cho.
However, she pointed out that only 5.2 percent of nursing hospitals for the elderly have set up an ethics committee. In comparison, 32.9 percent of all deaths occur at care hospitals, and 75.3 percent of nursing hospitals experience the occurrence of deaths.
There are also 12 public ethics committees for medical institutions that cannot have their own, and 106 medical institutions have concluded agreements with these public ethics committees.
The number of advance care registrations and their implementation totaled 80,298 from 2018 to 2021, and that of actual decisions on discontinuing life-sustaining care and their implementation totaled 192,456.
To reinvigorate the life-sustaining treatment decision system, Cho called for the government to obligate general hospitals to set up ethics committees, grant allowances to nursing hospitals to induce them to set up ethics committees, supervise medical institutions that have set up ethics committees but received no advance directives, relaxing rules for doctors’ decision on the discontinuation of life-sustaining treatment and strengthening the screening function of ethics committees.
In the following debate, various experts presented their views on improving the life-sustaining treatment decision system in the medical field.
Kim Myung-hee, head of the National Bioethics Policy Board, raised issues with adjusting the timing to discontinue life-sustaining treatment, the decision on the life-prolonging treatment of people without family or friends, reinvigorating the life-sustaining treatment decision system at nursing hospitals and educating medical workers on life-prolonging treatment decision system.
“The government needs to expand the targets of life-sustaining treatment discontinuation from dying patients to terminal patients, as are the cases in most foreign countries,” Kim said. “The timing of making advance directives is set at a terminal phase of disease now, but that also should be determined by physicians and patients in due course.”
Kim also suggested that the government should introduce an authorized agent system for patients without family and friends who have not prepared advance directives and allow only one doctor to decide on dying patients at nursing hospitals to reinvigorate the system at care hospitals.
“Lastly, the government needs to allow doctors at hospitals with ethics committees can confirm patients’ intention by checking the information system on life-sustaining treatment and introduce compulsory education of the system for medical professionals,” Kim added.
Professor Yu Shin-he of the Department of Palliative Care at Seoul National University Hospital cited as problems in the too-difficult process of deciding on life-sustaining treatment for patients, families, and medical workers, the sudden strengthening of self-determination rights for dying patients, lack of supportive care for patients and families, and the lack of a system that guarantees patients’ interests.
To resolve these problems, Professor Yu called for simplifying decision- making process, allowing medical workers to behave for patients if families oppose discontinuation of life-sustaining treatment against the will of patients, surveying and supporting medical workers’ care of dying patients, and introducing authorized agents aside from patients’ families in deciding the discontinuation of life-prolonging treatment.
“We hope the government will designate all medical institutions above the hospital level as registration offices of advanced directives because patients use these facilities most,” said Ahn Ki-jong, head of the Korea Alliance of Patients Organization. “Currently, families, not patients, make decisions concerning life-sustaining treatment more often. That must also change.”
Ahn said, “Five years have passed since the nation introduced the life-sustaining treatment decision system. However, there have been fewer cases of abusing the system than expected. Therefore, now is the time to reexamine it carefully from the viewpoint of patients. The system has also been many positive evaluations over the past five years, so the government should consider expanding its support.”

