Korea is almost the only country that recorded an increase in excess deaths during the Omicron wave due to its problematic critical care system bent only on making makeshift responses, an expert pointed out.

Professor Kim Young-sam of the Department of Pulmonology at Severance Hospital made these and other points at a joint online forum, “Continuous occurrence of Covid-19 patients and countermeasures for autumn” on Monday.
Kim analyzed the monthly excess deaths from Covid-19 from 2021 to May 2022 and found that Korea registered more than 18,000 excess deaths in March 2022 when the daily virus cases exceeded 600,000 and severe and critical cases hovered above 1,000. The number of Covid-19 deaths totaled 44,487 in March, 18,068 more than the expected deaths of 26,419.
In April, too, there were more than 10,000 excess deaths. Quarantine officials had predicted 26,320 deaths but the actual number totaled 36,697, he said.
“Korea had a lot of excess deaths from August 2021 to May 2022. These refer to all deaths – those from Covid-19 and other causes,” Professor Kim said. “The country marked the largest excess death during the peak of the Omicron wave in March 2022, with about 18,000 excess deaths. About half of them were due to Covid-19.”
Comparisons of excess deaths
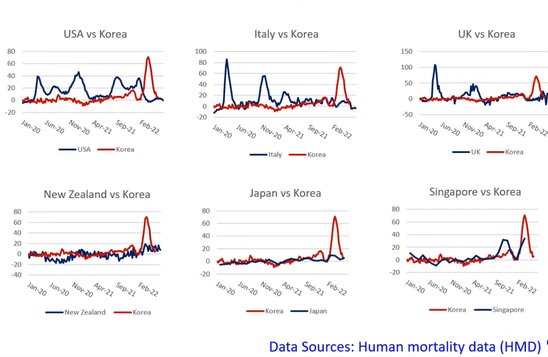
The Severance professor noted that compared to other industrial countries, Korea was almost the country that recorded an increase in excess deaths during the Omicron wave, showing a different pattern from other countries.
Kim also pointed out that the Covid-19 pandemic caused damage to non-Covid-19 patients by not receiving treatment on time.
According to his analysis of medical expenses for health insurance, the number of people hospitalized due to pneumonia totaled 314,775 in 2019, but the figure plunged to 183,157 in 2020 when Covid-19 began to spread and to 126,753 in 2021. Also, the number of deaths from ischemic heart disease per 100,000 people was 2.01 in August 2019, but it rose to 2.33 in August 2020. “We can presume that non-Covid-19 patients’ medical access dropped from this data,” Professor Kim said.
He noted that the index that can predict excess deaths most precisely is the number of severely ill Covid-19 patients in hospitals.
“The number of excess deaths is more important than fatality rate, and the number of critical cases is more crucial than sickbed occupancy rate,” Kim said. “Excess deaths begin to appear when the number of hospitalized severely ill patients reaches 300 or more nationwide. If more than 1,000 critical patients are hospitalized, up to 2,400 excess deaths can occur per week.”
Professor Kim cited insufficient medical resources as the reason for increasing excess deaths in proportion to severe and critical cases. Due to the government’s administrative order to mobilize sickbeds at tertiary general hospitals, the number of intensive care units for non-Covid-19 patients declined, depriving them of opportunities to receive treatment.

Kim pointed out that some 466 ICU beds have been reduced for non-Covid-19 severe patients to support Covid-19 patients and the nursing workforce. “Mobilizing 1 percent of total beds at tertiary general hospitals is equivalent to 20 percent of total ICU beds,” he said. “As the large hospitals have no workforce, they have no choice but to reduce the number of general ICUs.”
As a result of surveying 21 general hospitals and tertiary general hospitals in December 2021, there were 212 physicians and 1,168 nurses who treated critical patients at 279 beds, according to Professor Kim. When calculating the shift into four groups, the guideline of the Ministry of Health and Welfare requires 2,009 nurses, meaning that these ICU units operated with only 58 percent of the required workforce, he added.
Besides, not all nurses who worked at these units were ICU nurses but those dispatched from other departments and general wards, Kim pointed out. As a result, the fatality of severe Covid-19 patients was higher than non-Covid-19 critical patients.
“Although hospitals have secured beds, they have made no changes in the treatment system of critical patients. The most crucial point is how to secure a workforce. The authorities need to think about this, and make fundamental solutions and changes,” Professor Kim said. “We have persistently asked for activating a control tower, including experts in critical patients, and establishing the bed allocation system for severely ill patients, but are still receiving messages through the Kakao Talk.”

