The Organization for Economic Cooperation and Development has advised Korea to increase the number of students admitted to medical schools and introduce a pay-for-performance system.
With the current healthcare system, the country cannot meet populating aging and medical needs for chronic diseases, it pointed out, while emphasizing the need to improve the long-term care system and strengthen home-based care services.
These and other recommendations were contained in the “OECD Economic Surveys: Korea 2022," released by the club of industrial countries on Monday. It is a biennial report based on the OECD secretariat’s comprehensive analysis and evaluation of member countries’ economic trends and policies along with its policy recommendation.
The OECD pointed out that although Korea built one of the best healthcare systems in a short period, it falls short of preparing for an aging society.
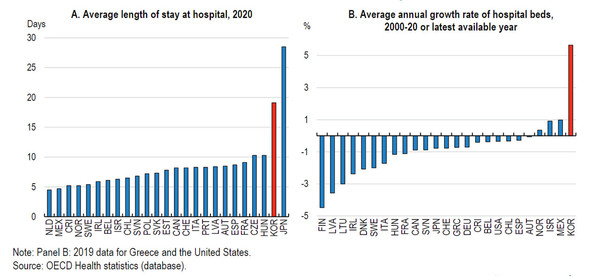
It then cited Koreans’ undue reliance on specialists and hospital care as structural problems. The average hospitalization period of Korean patients in acute care stood at 7.3 days, longer than the OECD average of 6.6 days. The number of hospital beds in Korea was 12.4 per 1,000 population, hovering far above the OECD average of 4.5.
Pointing out that Korea’s healthcare system overly relies on hospitalization and specialist care, the report said, “This overreliance is largely due to weak primary care, which does not function well enough as a gatekeeper authorizing specialist referrals and hospitalization.”
Korea’s fastest population aging in OECD means that a larger share of Korea’s population is likely to suffer from multiple chronic diseases, it noted.
“Primary healthcare with promising innovations and telemedicine can boost the capacity of the health system to contain and manage future health crises and reduce unnecessary hospitalization of people who can be effectively treated outside of hospitals,” it added.
The increase of doctors cannot be postponed anymore … general practitioners’ share should rise by introducing a pay-for-performance system
To strengthen primary care, the report said it is urgent to replenish general practitioners (GPs) who will provide primary care services.
It then advised Korea to increase the medical school enrollment quota and introduce the pay-for-performance system.
The share of GPs in Korea remains at 6 percent, far below the OECD average of 23 percent. The shortage is even more serious in Korea where the number of physicians per 1,000 inhabitants is smaller than other OECD members, according to OECD. The number of medical doctors per 1,000 people in Korea was 2.5, lower than the OECD average of 3.5. Accordingly, Korea needs to expand the number of admissions to medical schools and prepare for an aging society.
“Currently, Korean primary care is lacking in general practitioners. It will get even more serious soon, with many GPs nearing retirement and a declining number of new graduates specializing as GPs,” it said. “In 2020, the government decided to increase the number of admitted students in medical schools but it has been delayed due to Covid-19 and opposition from doctors’ associations. However, this should be implemented without further delays, in light of rapid aging.”

The OECD report advised the introduction of a pay-for-performance system to encourage applications for GPs. The scheme pays bonuses to physicians who achieve pre-defined targets, such as lower obesity rates, smoking cessation, and chronic disease management. Among OECD member nations, the U.K., the Netherland, and Portugal are implementing it.
The current fee-for-service scheme makes people prefer specialists. People tend to regard specialists provide higher-quality care than GPs, and think it's better to see a specialist if it's the same price, it said.
“Shifting away from the current fee-for-payment scheme while blocking patients from bypassing GPs when accessing specialists and hospitals could increase the attractiveness of the GP profession and better meet the challenges posed by an aging population and the rising burden of chronic conditions,” it said. “Studies suggest that the introduction of the pay-for-performance scheme in the United Kingdom is associated with higher retention of GPs, improved primary care quality, and increased job satisfaction.”
Long-term care reform will lower social hospitalization and reduce the elderly’s burden
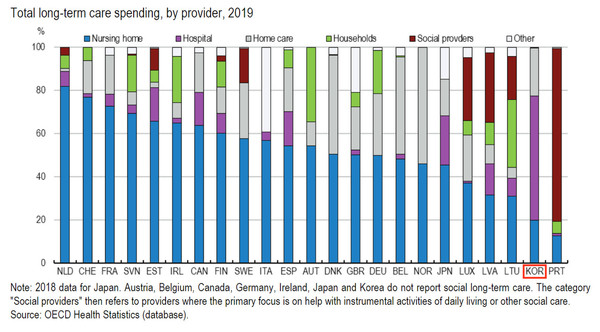
The OECD also emphasized the need to reform long-term care as the old-age safety net. As long as OECD sees it, Korea is a country that has a rare universal long-term care system but failed to prevent older adults from unduly resorting to hospitalization.
In Korea, the average length of stay per patient at long-term care (LTC) hospitals was 165 days in 2019, the longest among OECD member countries. The number of “social hospitalization” neared 170,000, accounting for 40 percent of total patients at LTC institutions.
This runs counter to the long-term care system’s objective of reducing the economic burden of elderly patients and preventing social hospitalization in LTC institutions for acute care. OECD cited as reasons the barren primary care environment, the insufficient connection between medical service and care, and the lack of low-cost home-based medical service.
“In Korea, using hospitals is financially more attractive for care recipients than using LCT institutions or homecare,” the report said. “While the national health insurance has a ceiling on co-payment according to income levels, the long-term care insurance does not. The flat-rate per diem reimbursement system should also be changed. The government should discourage private care providers and homecare medical service institutions from staging unsustainable and consumptive price competitions.”
The key to homecare lies in visiting nurse system … expanding their autonomy needed
OCED also cited the provision of high-quality homecare services as a major task. The report, while pointing out that “the lack of visiting nurse service was the primary cause of unmet needs in at-home healthcare,” called for expanding financial sources and securing the workforce.
In 2020, the proportion of visiting nursing services among all home medical services stood at only 1.6 percent. This contrasts with that 64.2 percent of long-term care recipients in Korea cited visiting nursing as the most essential service. Of the 20,000 people who needed visiting nursing services, only 7.4 percent could receive it.
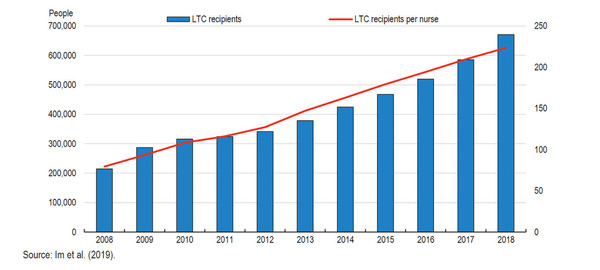
“Between 2010 and 2018, the number of long-term care recipients redoubled but that of nurses remained almost the same. About 74 percent of long-term care nurses are working part-time,” it said. “Low wages, poor working conditions, and insecure employment contracts are blocking the release of new nurses.”
The OECD report also advised expanding the autonomy of nurses in care and treatment.
“It is difficult for nurses in Korea to provide treatment autonomously. Regulations restrict nurses from treating patients according to their best judgment," it said. “It is necessary to strengthen the autonomy of nurses in the care field and increase economic benefits. In Scandinavian countries, highly educated nurses could increase their role by having greater autonomy at work.”

