India takes the lead in non-face-face treatment by running ‘state-run platform’

There are countries where telemedicine has become a necessity, not an option.
Some Asian countries, worried about the gap in medical infrastructure between regions, see telemedicine as a breakthrough. For instance, telemedicine has become a new routine in Vietnam with active participation by medical institutions. India also seeks to bridge the social and economic gap by operating a state-run telemedicine platform.
In the online academic conference organized by the Korean Telemedicine Society, telemedicine experts from Asia gathered together to share their countries’ current status of telemedicine and sought directions for development.
In Vietnam, where medical gaps are still wide among different regions and medical institutions, the government is making all-out efforts to introduce digital healthcare along with the development of information and communication technology (ICT). Amid this trend, interest in telemedicine has increased, and on the occasion of the Covid-19 pandemic, the Southeast Asian country revised its medical law to allow telemedicine temporarily.
As a result, about 8,000 institutions provided telemedicine, providing more than 3 million treatment services as of June.
“The key lies in the connection between higher and lower-level medical institutions. The central hospital plays a big role in providing medical treatment, surgical cooperation, and educational programs for other medical institutions remotely,” said Hieu Lan Nguyen, director of Hanoi Medical University Hospital. “Now, telemedicine has become a new normal in intensive care units of Vietnamese hospitals."

Thirty institutions are now playing a pivotal role as the central hospitals. Hanoi Medical University Hospital is one of them. One hundred and twelve medical institutions participate in the hospital’s telemedicine system. Twelve new treatment centers also opened to provide telemedicine exclusively by connecting to the hospital’s medical staff.
“Despite the rapid growth, telemedicine services are still limited. Like Korea, Vietnam has tasks to solve in law and institutions. We are also concerned about creating an economic compensation structure for remote cooperation and telemedicine. However, the government has a strong will to develop the telemedicine system. Therefore, we expect institutional problems to be resolved quickly."
India built a state-run telemedicine platform to solve socio-economic problems

In some countries, governments have built their telemedicine infrastructure. One such country is India, where medical infrastructure is extremely concentrated in cities.
According to Shashi Gogia, president of the non-profit Society for Administration of Telemedicine and Health Care Informatics (SATHI), India’s healthcare vacuum in rural areas has even aggravated since 2005, 17 years from now.
The unfulfilled rate of doctors at primary medical institutions in India rose from 17.5 percent to 21.8 percent. The situation is even more serious in special care. The unfulfilled rate of medical specialists at provincial medical institutions jumped from 47.7 percent in 2005 to 68.0 percent 17 years later.
“More than two-thirds of the Indian people live in provinces, but medical infrastructure has not improved as much as in urban areas. Even skilled physicians don’t want to work in provinces where infrastructure is poor, suffering from the shortage of basic equipment, including the X-ray machine,” Gogia said.
There is a more than 100 times cost gap for the same treatment between rural and urban medical institutions. Nor can people ignore the expenses for transport. Some statistics show that patients in rural areas must wait an average of 1.5 years and travel 1,000 kilometers to receive treatment from specialists. Nevertheless, people stop working and go to a specialist in the city “without eating or sleeping properly” for days.
All these explain why telemedicine is regarded as belonging to socioeconomic areas beyond medical care. Telemedicine reduces medical expenses. People don't have to travel hundreds of kilometers to get medical treatment and can continue their work, the SATHI president said.
“Regional healthcare quality is also improved. Provincial doctors can build up their skills through remote collaboration or education. It can also provide immediate help to the patient in an emergency," Gogia said. “Overall, the scope of medical services will expand."
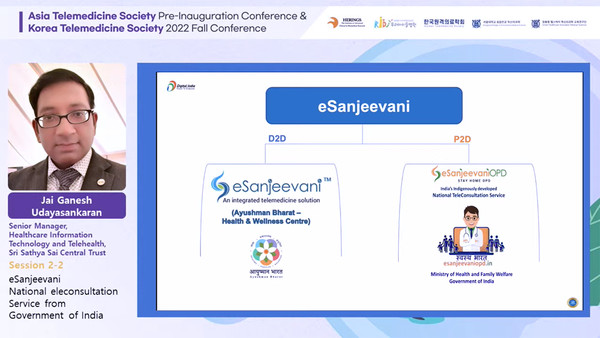
The Indian government launched the state-run telemedicine platform, eSanjeevani, in 2018. Run by the Ministry of Health and Welfare, eSanjeevani provides remote cooperation services between doctors and doctors and telemedicine services between doctors and patients. Medical staff training is also being conducted here. Through the platform provided by the government, doctors conduct real-time video treatment and make prescriptions. The medical data accumulated here is also reflected in the government's health care policy.
The platform rapidly grew as the world underwent the Covid-19 pandemic. The number of remote, cooperative treatments has totaled 58.6 million since 2018. A total of 181,883 Indian doctors registered with it, and 30,836 physicians are also operating in eSanjeevaniOPD, a platform for at-home care.
“About 67 million patients had received help from this service until September. We aim to help all of the 1.3 million Indians enjoy the benefit of digital health infrastructure,” said Jai Ganesh Udayasankaran, senior manager of Healthcare Information Technology and Telehealth. “With eSanjeevani, patients can access professional healthcare more easily and conveniently and receive uninterrupted care.”

