A research team, consisting of researchers from the Institute for Basic Science (IBS) and Chungnam National University (CNU), identified the cause of the inaccuracy in the drug interaction prediction formula recommended by the U.S. Food and Drug Administration (FDA).
According to the team, led by Professors Kim Jae-kyung at IBS and Chae Jung-woo and Kim Sang-kyum at CNU, drugs absorbed into the body are metabolized by enzymes in various organs, including the liver, and disappear from the body.
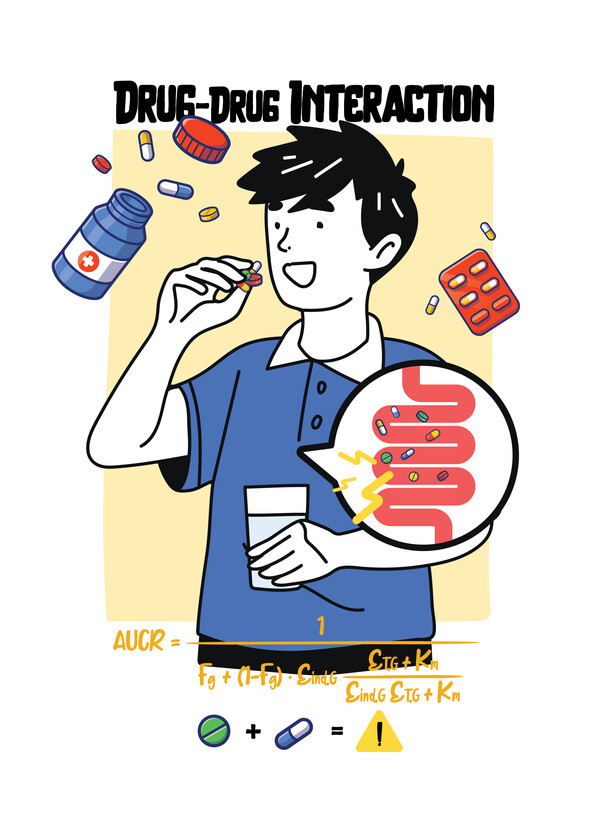
When two or more drugs are taken together, one drug may alter the metabolism of the other drug to promote or inhibit excretion in the body, and there is a possibility that the targeted treatment effect may not be achieved or side effects may occur, called drug-drug interactions (DDI).
Accurately predicting drug elimination rates according to DDI is very important for drug prescription and new drug development.
When prescribing a combination of drugs, a doctor makes a prescription based on the DDI information specified in the drug instruction manual.
In the process of developing new drugs, companies need to research and label DDI.
As a result, the FDA first issued guidance in 1997 (revised in January 2020) to evaluate DDI and minimize the side effects of multiple drug administration.
Since it is practically impossible to evaluate both new drug candidates and all marketed DDIs during the new drug development process, the FDA recommends indirectly evaluating DDIs using the formula suggested in the guidance.
However, the problem is that the accuracy of this formula is poor.
The formula proposed by the FDA is the Michaelis–Menten kinetics formula, which describes the reaction rate of enzymes, was first presented in 1913 and has been cited in more than 220,000 papers to date.
This formula presupposes that the concentration of enzymes in the body involved in drug metabolism is low.
The research team found the cause of the inaccuracy of the existing FDA formula by confirming that the concentration of enzymes involved in drug metabolism in the actual liver was more than 1,000 times higher than the value used for prediction.
Using the research results, the team developed a new formula that can explain drug interactions through a mathematical-pharmacy collaborative study.
Instead of the existing formula, which has been used without question, the team came up with a new formula that can accurately predict the drug metabolism rate regardless of the concentration of the enzyme.
Afterward, the team predicted DDI using the newly written formula and compared it with values measured in actual experiments.
As a result, the team confirmed that the prediction accuracy more than doubled without artificial correction.
The existing FDA formula predicted DDI within a 2-fold margin of error at 38 percent, whereas the revised formula reached 80 percent.
“Improving the accuracy of DDI prediction will contribute to increasing the success rate of new drug development and drug efficacy in clinical practice,” Professor Kim Sang-kyum said. “As the paper was published in the best clinical pharmacology journal, we expect that the FDA guidance will be revised according to the results of this study.”
Professor Kim Jae-kyung also said, “Thanks to the collaborative research between mathematics and pharmacy departments, we were able to correct the formula that we thought was the right answer for a long time.”
Kim stressed that he hopes that a formula developed by Korean researchers will be included in the FDA guideline.
The research, titled "Beyond the Michaelis-Menten: Accurate Prediction of Drug Interactions through Cytochrome P450 3A4 Induction," was published in Clinical Pharmacology and Therapeutics on Dec. 15.

