Song Kyo-young, professor of gastrointestinal surgery at Seoul St. Mary’s Hospital
A vital step in treating stomach cancer is the surgical removal of the cancerous tissue. However, to ensure complete removal of the cancer, it is often necessary to remove a significant portion of the stomach, resulting in uncomfortable symptoms.
Individuals with gastric cancer, especially those who have a habit of consuming large meals, may experience discomfort such as dumping syndrome, diarrhea, and abdominal pain if they fail to regulate their eating habits post-surgery. This often leads to readmission to the hospital. Consequently, endoscopic resection, which removes the cancer while preserving the entire stomach, is a desirable alternative.
Endoscopic resection is a minimally invasive procedure that uses an endoscope to remove cancerous lesions from the stomach. This breakthrough treatment can be performed under sedation or local anesthesia, eliminating the need for general anesthesia. After the procedure, most patients can return to their daily routines within a few days since the stomach tissue is almost completely restored to its original state.
In addition to removing the stomach, it's important to completely resect the lymph nodes around the stomach, as this is where stomach cancer metastasizes in the early stages of the disease. Endoscopic resection omits procedures outside the stomach, such as lymph node dissection, and is therefore only performed when it is determined that there is no chance that the cancer has spread to the lymph nodes around the stomach.
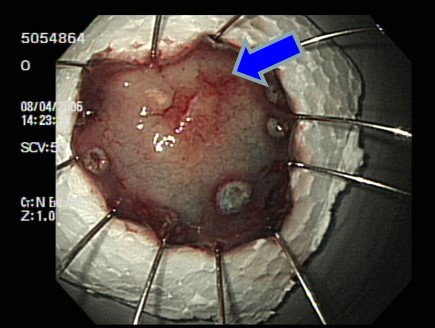
Endoscopic resection was initially reported in Japan in 1974 using the polypectomy technique, and it was known as endoscopic mucosal resection (EMR). In the late 1990s, with advancements in endoscopic instruments and techniques, a more effective endoscopic procedure was developed to remove stomach cancer by removing the submucosal layer of the stomach. This new technique is called Endoscopic Submucosal Dissection (ESD).

With the advent of ESD, larger cancers and those in difficult locations can be resected, expanding the range of gastric cancer patients who are candidates for endoscopic resection.
Endoscopic resection is a viable option only for patients with gastric cancer who do not have lymph node metastasis. Pathology reports of a significant number of patients who underwent surgery for gastric cancer were analyzed to determine the factors associated with lymph node metastasis. Four factors were identified: 1) depth of cancer, 2) degree of differentiation, 3) size of the tumor, and 4) presence of ulceration.
In other words, if the cancer is very thin (confined to the mucosal layer), well differentiated, small (2 cm or less), and ulcer-free, there is no lymph node metastasis and endoscopic resection is possible.
This is referred to as an “absolute indication.” If the patient meets the criteria, endoscopic resection is recommended rather than surgical resection.
Numerous studies have been conducted since then, demonstrating that endoscopic resection can be performed in situations where the risk of lymph node metastasis is relatively low, despite the absolute indication being slightly higher. The following are some notable examples:
1) Cancers larger than 2 cm are acceptable if they are ulcer-free, confined to the mucosa, and well differentiated.
2) If ulceration is present, but well-differentiated, cancers smaller than 2 cm in size are acceptable.
3) Cancer that has invaded the submucosal layer but is not deeper than 500 micrometers is acceptable if it is well differentiated and is 3 cm or less.
4) If it is 2 centimeters or less with invasion only to the mucosal layer, it is possible, although the differentiation is poor.
These criteria are called extended criteria. While the expanded criteria for endoscopic resection is good news for patients, it is not yet the standard of care.
The frequency of lymph node metastasis in different studies has varied between researchers, the accuracy of preoperative tests is not perfect, so the actual results after the procedure may be different, and long-term follow-up results are still lacking.
In particular, poorly differentiated gastric cancer, including ring cell cancer, has a higher rate of lymph node metastasis than other cancers, even if it is small and shallow, so further research is still needed. And we should wait for the results of actual clinical trials.
Compared to open surgery, endoscopic resection has several advantages, including not requiring general anesthesia, lower complication rates, and higher patient satisfaction. These benefits make it a suitable option for elderly patients who are at an increased risk for complications due to surgery or general anesthesia, as well as for high-risk patients with multiple medical conditions.
It is important to note that if the test results show that the patient is outside of the absolute or expanded indications, or if the pathological examination following the procedure reveals results that do not meet the standard criteria, surgery should be considered as a follow-up treatment. Additionally, if complications such as bleeding or perforation occur during the procedure, consultation with a surgeon is necessary to determine whether surgery is required.
This article was originally published in Korea Healthlog, a sister paper of Korea Biomedical Review, on April 3. -- Ed.

