Teva Handok's severe asthma treatment Cinqair (reslizumab) crossed the threshold of the Drug Benefit Evaluation Committee (DBEC) Thursday, six years after it won approval from the Ministry of Food and Drug Safety.
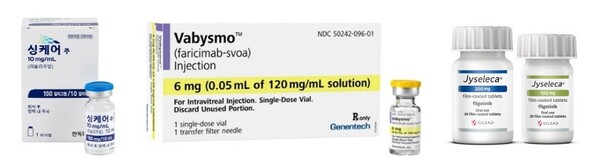
The seventh DBEC meeting this year also recognized the appropriateness of reimbursement for Roche Korea’s Vabysmo (faricimab), the first bispecific antibody treatment for ophthalmic diseases, and Eisai Korea’s Jyseleca (filgotinib), the oral Janus Kinase (JAK) inhibitor, if they accept amounts below assessment.
According to the Health Insurance Review and Assessment Service (HIRA), Teva Handok’s interleukin-5 (IL-5) inhibitor Cinqair won recognition for its appropriateness in treating severe eosinophilic asthma. It has been six years since the ministry approved the drug in September 2017.
According to WHO's announcement, Korea has the second highest asthma mortality rate in the world and urgently needs to treat and manage severe asthma patients. However, the use of biologics, which can reduce steroid use in severe patients and healthcare costs resulting from repeated hospitalizations, has been extremely limited.
The only biologic available for prescription for severe asthma is Novartis' Xolair (omalizumab), approved in 2007. However, it is usable only for allergic asthma, leaving no reimbursed biological drugs for eosinophilic asthma with a poor prognosis.
So far, the food and drug safety ministry recognizes four biologics as eosinophilic asthma treatments. The four are Cynqair, GSK's Nucala (mepolizumab), AstraZeneca's Fasenra (benralizumab), and Sanofi's Dupixent (dupilumab), and three of them are undergoing insurance benefits review by HIRA.
Therefore, interest is rising in whether Cinqair will become the first eosinophilic asthma treatment to be approved for reimbursement in Korea as it crosses the threshold of DBEC.
Cinqair awaits a drug price negotiation with the National Health Insurance Service (NHIS) and will receive reimbursement through the Health Insurance Policy Review Committee (HIPRC)’s decision.
The DBEC recognized Roche's Vabysmo and Eisai's Jyseleca as affordable on the condition that the drugmaker accept a drug price below the review committee's assessment.
Vabysmo is an intravitreal injection approved earlier this year to “treat neovascular (wet), age-related macular degeneration" and "treat vision impairment due to diabetic macular edema.”
While the existing treatments, such as Bayer’s Eylea (aflibercept) and Novartis’ Lucentis (ranibizumab), and Beovu (brolucizumab) are vascular endothelial growth factor (VEGF) inhibitors that share the same mechanism of action, Vabysmo targets both VEGF-A and Ang-2 simultaneously to block pathogenesis more comprehensively. It also improves patient comfort with intravitreal injections by extending the dosing interval to up to four months.
Jyseleca won a nod in April last year to treat rheumatoid arthritis and ulcerative colitis. It is the fifth oral JAK inhibitor introduced in Korea, following Pfizer's Xeljanz (tofacitinib) and Cibinqo (abrocitinib), Lilly's Olumiant (baricitinib), and AbbVie's Rinvoq (upadacitinib).
On the other hand, Meditip's rare cancer drug Yondelis (trabectedin), which crossed the threshold of the Cancer Disease Review Committee in May, was decided as reimbursable after deliberations by the DBEC.
Yondelis, approved to treat soft tissue sarcoma in 2008, had suspended and resumed its sale in Korea. Meditip made a renewed attempt for reimbursement 15 years after it won a nod from the ministry but failed to cross the threshold.
Roche's RET inhibitor Gavreto (pralcetinib), was also denied coverage by the committee. Gavreto failed to meet the criteria for reimbursement in the cancer review committee in June and was confirmed as non-reimbursable at the DBEC review.
Roche recently returned the rights for Gavreto to the original developer, Blueprint Medicines Corp., and will discontinue the sale of Gavreto in Korea at the end of this year.

