After undergoing five open heart surgeries for congenital heart disease, a patient successfully received a heart transplant and now leads a healthy life without experiencing any rejection.
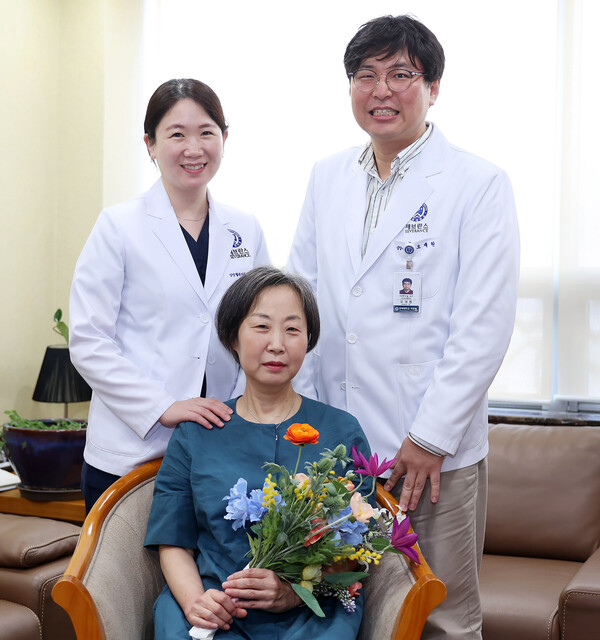
The medical team of Professor Shin Yu-rim of cardiovascular surgery and Professor Oh Jae-won of cardiology at Severance Cardiovascular Hospital said on Friday that they performed a successful heart transplant on Oh Mi-hye Oh, a 62-year-old woman with blood type O, who had previously undergone five thoracotomies for congenital heart disease.
Six months after the transplant, she is in a healthy condition without any rejection, the hospital said.
In 1972, during her sixth-grade year, Oh underwent corrective surgery at Severance Hospital to address Tetralogy of Fallot (TOF), a congenital heart defect that disrupts normal blood flow through the heart.
TOF is a complex condition characterized by the simultaneous presence of four heart abnormalities: ventricular septal defect, right ventricular outflow tract stenosis, overriding aorta, and right ventricular hypertrophy. Without surgical intervention, TOF carries a high mortality rate, and the surgical procedure itself poses significant challenges. Approximately 5-7 percent of all patients with congenital heart disease are affected by TOF.
Despite undergoing surgery for TOF, Oh experienced additional challenges and had to undergo four more open-heart surgeries, which included ventricular septal defect repair and pulmonary artery valve replacement, until 2007.
Following these surgeries, she was able to live a relatively uneventful life.
However, in October 2020, her shortness of breath worsened, leading her to seek medical attention at Severance Hospital.
Subsequent tests showed both left and right ventricular failure. Despite receiving a cardiac stimulant, her shortness of breath continued to worsen, and her edema intensified. Eventually, her condition progressed to end-stage heart failure, requiring a heart transplant.
She was put on the heart transplant waiting list and admitted to the hospital in January 2021.
However, finding a suitable donor heart was difficult. Being a blood type O patient, she faced a comparatively longer waiting period for a suitable donor in comparison to individuals with other blood types. Additionally, Oh was classified as "highly sensitized," indicating that her antibodies reacted with a significant portion of the antigens during the histocompatibility antibody screening test conducted prior to transplantation.
Specifically, being highly sensitized meant that there was a greater likelihood of her antibodies attacking the transplanted organ and triggering acute rejection.
Her medical team used medication and plasma exchange to lower her antibody levels while waiting for a suitable donor heart.
However, in December 2022, Oh's condition worsened, leading to the decision of placing her on extracorporeal membrane oxygenation (ECMO). ECMO treatment involves the insertion of a thick conduit into a blood vessel to provide mechanical assistance to the weakened heart. Typically, patients undergoing ECMO are kept in a sedated state and receive ventilator support, with the conduit inserted through a leg vein.
However, due to Oh's long hospitalization and severe heart failure, prolonged sedation could weaken her muscle strength and negatively impact her post-transplant outcome. To maintain her muscle strength, Professor Shin who performed the transplant surgery, kept her awake without a ventilator and maintained ECMO using only the blood vessels in her upper extremities, waiting for a donor heart to come along.
In January 2023, about a month after starting ECMO, the patient underwent heart transplant surgery.
Due to blood vessel adhesions from multiple open-heart surgeries and her unusual heart shape, her surgery took more than eight hours.
Eventually, Oh's surgery was successful. The hospital reported her discharge without any complications, and she is now leading a normal life.
When a patient undergoes a transplant surgery, his or her health is checked at six months and one year post-operatively to ensure that the transplanted heart is not rejected.
Oh underwent an autoantibody test and echocardiogram six months after her heart transplant. The antibody test showed no antibodies attacking the donor heart and no rejection.
"She was a difficult patient with a very long waiting period for heart transplantation as a blood type O recipient with multiple heart surgeries and dysfunctional left and right ventricles, and a high rate of autoantibodies, so she was at high risk of rejection," said Professor Oh. "We were able to achieve a positive outcome because the patient and her guardian trusted and followed the medical team even under difficult circumstances."
Related articles
- Severance introduces smart bed management system for efficient room occupancy
- Patient with 10 times normal liver weight gets successful transplant at Severance
- Iron Child event inspires hope in pediatric heart failure patients
- Severance's new Aortic Center aims to detect cardiac diseases in 'golden time'
- Severance Hospital develops AI program to predict chronic kidney disease risk from retinal exams
- Kidney xenotransplant from pig to monkey shows promising 221-day survival record
- Clinical trials of xenotransplants scheduled to start in 2024 Q4 in Korea
- EyeGene’s myocardial ischemia drug fails to prove efficacy in domestic phase 2 trials

