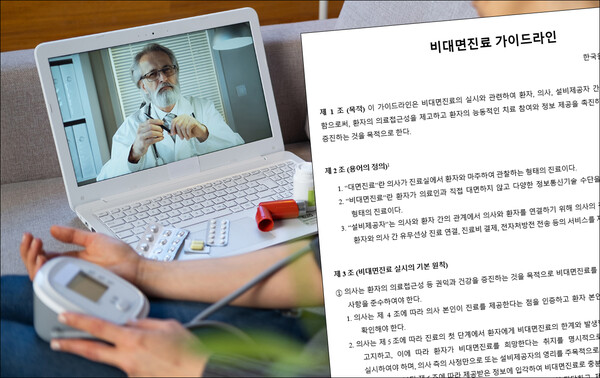
The medical community is preparing to institutionalize virtual care. A case in point is the issuance of “non-face-to-face medical treatment guideline.”
The Korean Telemedicine Society has come up with the guideline that contains basic principles and conditions for non-face-to-face medical treatment.
Notably, the guideline advised doctors to ask for patient consent before conducting a non-face-to-face consultation by telling them that doctors are not responsible even if uncontrollable medical accidents occur. In addition, it classified symptoms unsuitable for non-face-to-face treatment at each medical department, strictly limiting the provision of telemedicine care.
The society released its guideline for non-face-to-face medical treatment, containing these and other points on Wednesday. It also held a public hearing at the Seoul National University Cancer Institute in Jongno-gu, Seoul, to collect opinions on the guideline later in the day.
The guideline specified patient identification and notification of limitations and disadvantages as conditions for conducting non-face-to-face medical treatment. After verifying the patient's identity, doctors must notify them of non-face-to-face treatment's limitations and possible disadvantages.
Doctors should inform patients that the information they can obtain from non-telemedicine is limited due to the difficulty of auscultation, palpation, and examination and that diagnosis of serious diseases, such as tumors, infectious diseases, and cardiovascular diseases, may be missed if patients do not actively cooperate and provide information.
In addition, doctors must tell patients that information technology errors may cause interruptions or errors in non-contact medical treatment, but the physician is not responsible for this or liable for force majeure medical accidents.
Such notification can also be made through the provider's interface, and in case of emergency or time constraints, a virtual visit can be made without the patient's consent.
The guideline also includes a list of symptoms not suitable for first-time non-face-to-face consultation and that of medications that must be examined before prescribing. It also organized symptoms at each medical department unsuitable for telemedicine due to urgency, lack of information, or the means of responses.
The guideline also addresses medication delivery.
It defined companies that provide platforms for telemedicine or drug as "facility providers," obligating them to create an effective and safe environment. In particular, it stipulated that companies that provide drug delivery should establish a distribution network to ensure that drug delivery can be carried out quickly upon prescription.
The guideline also outlined how doctors can refuse to provide virtual care.
For instance, doctors can refuse telemedicine services if patients refuse or delay providing information to verify their identity or indicating a desire for telemedicine. Doctors can also refuse non-face-to-face treatment if they believe switching to an in-person visit and prescription is necessary.
However, the guideline emphasized that such a refusal must get an authoritative interpretation that it does not constitute a refusal of medical treatment under Article 15 of the Medical Service Act.
The society has made its guideline by referring to the guidelines released by the Telemedicine Research Society in April, the Korean Medical Association's "Guidelines for Telemedicine Pilot Project" released in May, the Japanese Ministry of Health, Labor and Welfare's "Guidelines for the Appropriate Implementation of Online Medical Care" revised in March, and the Japanese Federation of Doctors’ Associations’ "Recommendations for the Initial Consultation of Online Medical Care" prepared in 2021.
The Korean Telemedicine Society was launched in May 2021 as Korea's first academic organization specializing in telemedicine. It grew out of the Korea Telemedicine Research Association, founded in March of that year, and includes representatives from universities, hospitals, and industry.
Related articles
- Doctors call for permitting telemonitoring for arrhythmia patients
- Hospitals to check patients’ eligibility for remote care from next month
- Welt, Aimmed face delays in launching Korea's first approved DTx devices
- ‘More pilot projects needed to promote value of telemedicine in Korea’
- 57% of telemedicine prescriptions were non-reimbursed: survey

