Breast cancer patients are demanding insurance coverage for Novartis' Piqray (alpelisib) after it failed to meet the Health Insurance Review and Assessment Service (HIRA) Cancer Disease Review Committee's criteria.
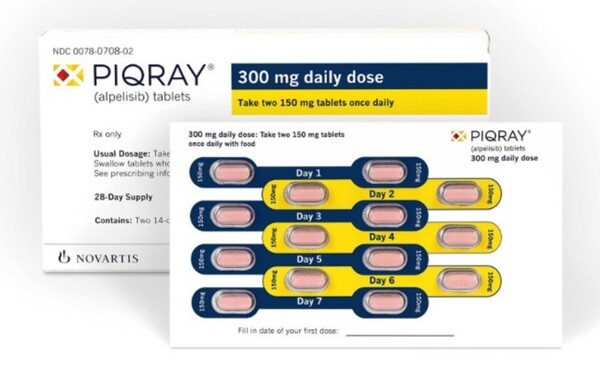
Piqray is a "PIK3CAα inhibitor" that blocks the excessive activity of the PI3K pathway by inhibiting the overactivation of PI3K-α caused by mutations in the PIK3CA gene.
It is a targeted anticancer agent used in combination with fulvestrant for previously untreated patients with hormone receptor-positive/human epidermal growth factor receptor-negative (HR+/HER2-) advanced or metastatic breast cancer.
PIK3CA mutations are frequent genetic alterations present in approximately 40 percent of HR+/HER2- advanced breast cancer patients, linked to resistance to endocrine therapy, disease progression, and poor prognosis.
Novartis sought reimbursement after gaining approval from the Ministry of Food and Drug Safety in May 2021 but failed to meet the cancer committee's requirements.

Recently, a message was posted on Petition24, a state online website, calling for the coverage of Piqray for breast cancer patients. The petitioner pointed out that although the drug has been touted as the only treatment for breast cancer patients with the PIK3CA gene mutation, its high cost prevents them from even trying it. The petition will be reviewed until Oct. 13 after collecting public opinions.
"My mother has stage 4 breast cancer, and there are not many medicines available," said a patient’s guardian. "As a last resort, she is taking Piqray. The problem is that this drug is not recognized as a reimbursable treatment, so she has been taking it for over a year and a half, paying more than 5 million won ($3,780) a month. The cumulative drug cost has approached 100 million won."
The poster pointed out that Qiagen Korea's PIK3CA companion diagnostic gene test reagent was also recognized as reimbursable. This is a recognition that PIK3CA expression is fatal for breast cancer patients, but Piqray is still marginalized, he added.
"Patients and their guardians are burning up. Due to the high cost of the drug, many breast cancer patients cannot try it and opt for the strong general chemotherapy, the petitioner said. Why should Korea follow suit long after safety has been proven overseas? It's hopeless," he said.
The petitioner reiterated his demand in conclusion.
"We strongly health authorities to cover the combination of Piqray + fulvestrant for patients with PIK3CA gene expression and who are not responding to CDK4/6 inhibitors," he said. "If this situation is prolonged, it will lead to financial ruin for families, and some patients will die without being able to try the drug due to the unaffordable cost."

