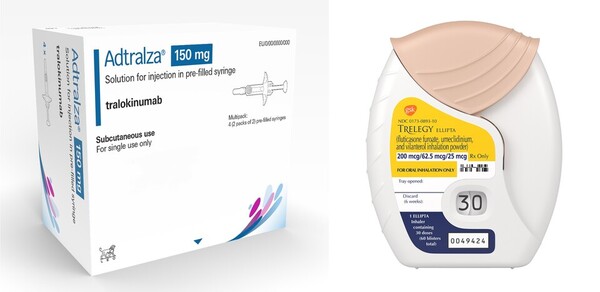
LEO Pharma's Adtralza (tralokinumab), the second biologic approved to treat atopic dermatitis, and GSK's Trelegy 200 Ellipta (fluticasone/umeclidinium/vilanterol), a triple inhaler asthma medication with an increased steroid dose, have won recognition for reimbursement.
In contrast, Antengene's Xpovio (selinexor) and Meditip's Yondelis (trabectedine) tried again to enter the reimbursement system but failed to cross the Pharmaceutical Benefits Evaluation Committee threshold.
The Health Insurance Review and Assessment Service (HIRA) released the results of the 12th meeting of the committee on Thursday.
Adtralza passed the committee less than three months at an ultrafast tempo, less than three months after it won the nod from the Ministry of Food and Drug Safety (MFDS).
Adtralza is a monoclonal antibody that selectively targets interleukin-13 (IL-13), which plays a key role in the immune and inflammatory processes underlying the signs and symptoms of atopic dermatitis.
In late August, it won MFDS’s approval for treating moderate to severe atopic dermatitis not adequately controlled by topical therapies in adults (18 and older) and adolescents (12 to 17 years) who are candidates for systemic therapy or for whom such therapies are not recommended.
Following Sanofi's Dupixent (dupilumab), it is the second biologic for treating atopic dermatitis, which simultaneously targets IL-4 and IL-13. For maintenance treatment, Adtralza can be adjusted to a four-weekly dosing interval, improving dosing convenience for patients compared to the two-weekly dosing interval of Dupixent.
Trelegy 200 Ellipta, a triple combination ICS/LABA/LAMA inhaler, has also won the committee’s recognition. GSK introduced it at the end of September last year, doubling the inhaled corticosteroid fluticasone content of the original Trelegy Ellipta.
Trelegy200 Ellipta is indicated for the "maintenance therapy of asthma that is inadequately controlled with a combination of long-acting beta2-agonists and inhaled corticosteroids in adults.
On the other hand, Antengene failed in its second attempt to reimburse Xpovio. It is an oral drug for treating relapsed or refractory multiple myeloma and diffused large B-cell lymphoma, and won MFDS approval in July 2021.
Antengene immediately applied for reimbursing Xpovio, tabling it on the Cancer Disease Review Committee's agenda in January 2022, but failed to establish coverage criteria in its first attempt.
Antigen then reapplied for the coverage of Xpovio in January this year, placing it again on the cancer review panel. However, it won only half success because it was covered for treating only multiple myeloma but not lymphoma indications. The subsequent reimbursement evaluation committee also made a “non-reimbursement” decision.
Yondelis also received a “non-reimbursement” decision from the evaluation committee this time, following a similar failure in July, failing in two attempts.
Yondelis, approved for treating soft tissue sarcoma in 2008, was suspended from domestic marketing and relaunched. Meditip challenged Yondelis' reimbursement 15 years after its approval by MFDS but failed to cross the threshold of the committee once again.

