A research team at the Korea Institute of Science and Technology (KIST), in partnership with Seoul National University (SNU) and Kyung Hee University, developed a new drug delivery system that could better treat retinal diseases.
Retinal diseases, such as age-related macular degeneration and retinitis pigmentosa, pose a serious threat to vision, often leading to blindness.
These conditions, caused by damage to the photoreceptor cells in the retina, have been challenging to treat effectively. Until now, the best available treatment involved frequent injections of anti-inflammatory drugs directly into the eye, a process that is both inconvenient and temporary.
The research team, led by Professors Im Mae-soon of the Brain Science Institute at KIST, Oh Seung-ja of the Department of Genetics and Biotechnology at Kyung Hee University, and Lee Kang-won of the Department of Applied Bioengineering at SNU, came up with a new treatment method by utilizing a substance that inhibits EZH2, an inflammation factor, as an anti-inflammatory agent.
According to the team, this is the first time EZH2, which accelerates retinal degeneration by triggering inflammatory responses in photoreceptor cells, has been targeted for treatment.
In a preclinical study involving rats with retinal degeneration, the injection of this anti-inflammatory slowed the progression of the disease.
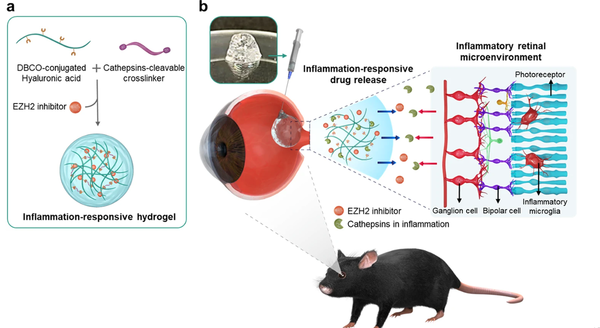
Also, the team developed a novel hydrogel capable of effectively delivering the anti-inflammatory drug to the site of inflammation.
This hydrogel, designed to slowly degrade in response to enzymes like cathepsin, which are overexpressed in inflammatory environments, successfully reduced inflammation levels in the retina by 6.1 percent when injected into rats with retinal degeneration.
It also demonstrated a protective effect on photoreceptor cells, reducing vision loss by up to four times compared to the control group.
A key feature of this new hydrogel is its base of hyaluronic acid, similar to the eye's vitreous body.
The teams stressed that this allows for the adjustment of drug degradation rates based on the individual patient's level of retinal inflammation, potentially minimizing the need for repeated injections, which could significantly reduce the economic and safety burdens for patients with mobility issues due to vision loss, and decrease the frequency of hospital visits for early-stage patients.
"We intend to further refine this technology by data-driven customization of the drug and hydrogel quantities and treatment cycles, as well as assessing the long-term stability of the drug delivery system," Professor Im said.
Professor Oh also said, "Our next step is to explore the application of this reactive drug delivery system to a wider range of ophthalmic diseases beyond retinal degeneration, by investigating various inflammatory and other factors involved in these conditions."
The research results were published in the npj Regenerative Medicine.

