Long-term sodium-glucose transport protein-2 (SGLT-2) inhibitor treatments in type-2 diabetic patients have reduced estimated glomerular filtration rate (eGFR) in “some” patients. Based on these results, two medical societies recently recommended doctors to prescribe SGLT-2 inhibitors while keeping monitoring the eGFR.
The recommendation came at an online symposium jointly organized by the Korean Diabetes Association (KDA) and the Korean Society of Nephrology (KSN), on Friday.
As many studies recently proved SGLT-2 inhibitors’ cardiovascular benefits in type-2 diabetes, researchers are paying attention to the drugs’ effect not only on the heart but the kidney. Against this backdrop, the two societies made the treatment guidelines after reviewing studies on their impact on protecting the organ.
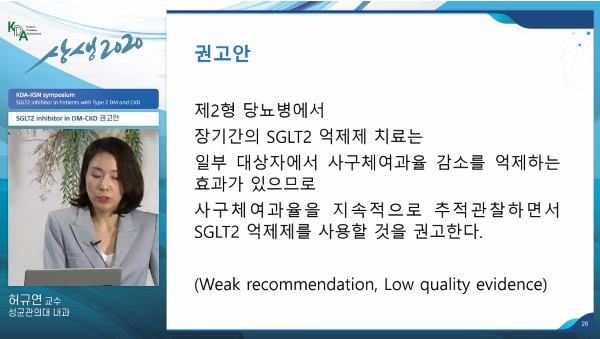
The key discussion during the online event was on whether the long-term use of an SGLT-2 inhibitor would help type-2 diabetic patients recover renal functions. The two societies concluded that “it was effective to preserve renal functions in some patients.”
However, they set the recommended strength and the evidence level as “weak” and “low,” respectively.
Hur Kyu-yeon, a professor at the Endocrinology and Metabolism Department of Samsung Medical Center, said related clinical studies were well-planned. Still, many patients discontinued participation in the long-term follow-up.
“In the final stage, the studies could not be maintained to be concluded,” she said during the online conference. “Although most of the literature was Western-oriented studies, the effect was different between Westerners and Asians. We made such a decision because long-term studies in Asians were needed.”
The societies’ meta-analysis on studies included those on dapagliflozin, empagliflozin, ipragliflozin, and ertugliflozin available in Korea, among randomized, controlled trials on SGLT-2 inhibitors with more than 52 weeks and more than 100 patients published between January 2015 and March 2020.
Out of the total 14 trials, 10 were about clinical data on dapagliflozin and empagliflozin. The analysis was made centering on eGFR figures.
After the announcement of the recommendations, panelists said they felt sorry that the recommendation level was “weak” and that there were no detailed guidelines for the use of SGLT-2 inhibitors depending on different levels of the renal functions.
Kwon Hyuk-sang, director for the KDA’s medical training affairs, who is also a professor of the Endocrinology and Metabolism Department at Yeouido St. Mary’s Hospital, said he was glad that the KDA inserted SGLT-2 inhibitors’ renal benefits in the latest treatment guidelines for diabetes.
However, it would have been better if the KDA had detailed the effect of SGLT-2 inhibitors depending on levels of renal diseases, he noted.
Professor Kim Nan-hee of Endocrinology Department of Korea University Ansan Hospital pointed out that the reviewed literature did not include studies on canagliflozin, which showed renal effects of SGLT-2 inhibitors well.
Kim Tae-hee, a professor of the Internal Medicine Department at Busan Paik Hospital, said the latest recommendations were based only on eGFR figures, while albuminuria is regarded as an alternative indicator of the progression of the renal disease.

