“The combination of atezolizumab and bevacizumab is the first immune-based combo therapy that beat sorafenib in the IMbrace150 study. Compared to sorafenib, the combo treatment showed better overall survival (OS) and progression-free survival (PFS). The combo not only improved objective response rate but extended the duration of response significantly. This is very encouraging in liver cancer treatment.”
Yu Su-jong of the Gastroenterology Department of the Liver Cancer Center at the Seoul National University Hospital (SNUH), made this and other remarks on the study of the Tecentriq plus Avastin combo during a YouTube show on Medical Library, a channel for healthcare professionals operated by The Korean Doctors’ Weekly.
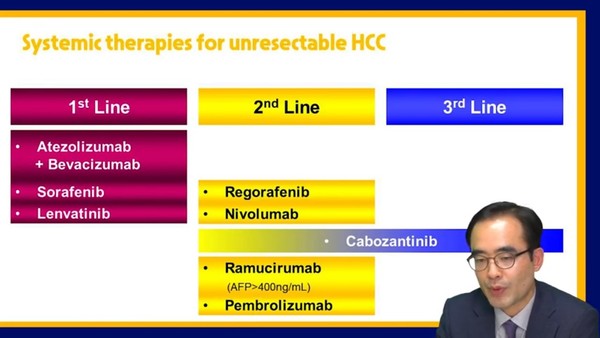
According to Yu, treatments for hepatocellular carcinoma (HCC) have progressed from cytotoxic drugs to tyrosine kinase inhibitors (TKIs) since 2000. In 2011, the era of immune checkpoint inhibitors (ICIs) opened. Most recently, the era of immune-based combination therapy mixing effective treatments such as ICI and TKI has come, he explained.
The most exemplary treatment option that prompted immune-based combo treatment for the first-line treatment of HCC was the use of Roche’s Tecentriq (atezolizumab), anti-PD-L1 immunotherapy, and Avastin (bevacizumab), a vascular endothelial growth factor (VEGF) inhibitor, Yu said.
Roche disclosed the results of the IMbrave150 study where the systemic therapy beat sorafenib for the first time, Yu said.
“The study compared the combo of atezolizumab and bevacizumab with sorafenib, head to head, and set the primary outcome as OS and PFS,” he said. “The combo group showed a meaningful improvement in survival and has not reached the median OS yet, showing an excellent survival extension.”
The results of the OS subgroup analysis demonstrated that among the groups with low initial alpha-fetoprotein (AFP) levels, extrahepatic spread (EHS), or macroscopic vascular invasion (MVI), the combo treatment group showed a more significant improvement in survival, compared to the sorafenib group, Yu said, adding that it will be worth considering this as a marker in patient selection.
In terms of PFS, 55 percent of the combo group did not have progression at six months, versus 37 percent of the sorafenib group.
“In particular, the ORR was significantly high in the combo group whose ORR improved up to 30 percent. But in the sorafenib-treated patients, the figure was only 11 percent,” he said.
Yu emphasized that what matters is how long such a good treatment response will last. While the sorafenib group’s median duration of response was only 6.3 months, the combo group did not yet reach the median value, indicating that the ORR continued for a considerable time.
People might worry about the safety of combo therapy because the treatment was highly effective. However, the two groups did not show a significant difference in adverse events that were so serious that the researchers had to stop treatment.
“As the study used VEGF inhibitor bevacizumab, there was great concern about major bleeding. But the two groups showed little difference in upper gastrointestinal bleeding – 7 percent versus 4.5 percent,” he said.
Yu noted that the IMbrave150 study enrolled patients after performing ligation to those who had variceal bleeding risk in the endoscopic screening within the past six months. Therefore, when treating a patient, a physician should first study variceal bleeding risk to perform an endoscopic variceal ligation (EVL), he said.
In the first-line treatment of HCC, the Korean regulator approved atezolizumab in combination with bevacizumab in late July, following the nod for the traditional therapy sorafenib and lenvatinib, which was non-inferior to sorafenib, according to Yu. “It is very encouraging that there are more first-line treatment options for HCC,” he said.
However, as the national health insurance cannot cover the combo treatment, an HCC patient should spend about 450 million won ($386,985) to 500 million won per month to receive the therapy, making it difficult to choose the combo treatment.
“The government says it would allow reimbursement only when the company submits valid data. But we are fighting a formidable enemy, liver cancer. So, I hope they can trust doctors’ independent judgment without being too obsessed with evidence,” Yu said.
On Wednesday, The Korea Doctors’ Weekly, the sister paper of Korea Biomedical Review, uploaded a medical review on “Opening a New Era in Hepatocellular Carcinoma Treatment,” the first video clips of the Liver Week 2020, held online from Aug. 13-14.

