“Half of the Korean patients with atrial fibrillation (AF) are taking low-dose non-vitamin K antagonist oral anticoagulants (NOACs), and half of them are underdosing. Unlike apixaban and edoxaban that reduced the doses in half, rivaroxaban 15mg has shown consistent efficacy and safety, as much as the 20mg standard dose. So, it can be used without concerns for underdosing.”
Professor Shim Jae-min at the Cardiology Division of Korea University Hospital said this and other remarks during his presentation, “What is the Optimal NOAC for Korean NVAF (non-valvular atrial fibrillation) Patients with Specific Considerations,” at the autumn academic conference of the Korean Society of Cardiology on Sunday.
Recently, European guidelines no longer put NOAC and warfarin in the same class and recommended that physicians should use NOAC first as Class 1 to prevent stroke in AF patients, Shim said.
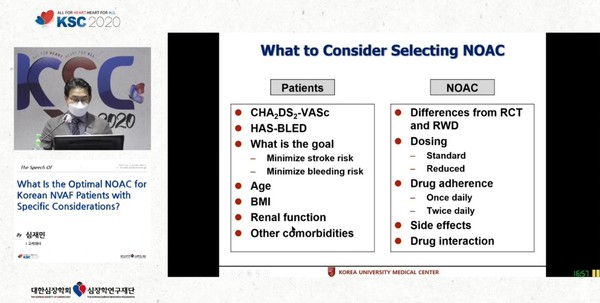
As NOACs are divided depending on patients' and agents' characteristics, it was important to choose which drug in which patients, he emphasized.
When prescribing a NOAC, physicians find it difficult to determine the dose and keep the standard perfectly in real clinical settings, he went on to say. This is why most doctors prescribe overdosing or underdosing of NOACs, he said.
Shim recently published a study on stroke prevention and bleeding safety in Korean patients treated with Xarelto (ingredient: rivaroxaban). He was the first author of the XANAP Korea study. Through his presentation on Sunday, he emphasized that Xarelto was useful for Korean patients.
XANAP Korea is the first Korean data analysis of the XANAP study, where Xarelto proved consistent efficacy and safety through future real-world research in Asian clinical settings. Shim explained that 35 percent of the 844 Korean patients included in the analysis used a low dose of Xarelto 15mg and produced positive results despite the low dose.
Korea Biomedical Review met with Shim to learn what the XANAP Korea study meant, what kind of implications its data offered, and Xarelto’s advantage to decide the dose of NOACs in Korean patients.
Question: As the first author, can you explain the significance of the XANAP Korea study?
Answer: First of all, the study design was prospective. There have been many real-world studies on NOACs recently, but all of them were retrospective. Unlike analyzing old data, the XANAP study was a prospective one.
Retrospective studies are bound to have a lot of missing data. Those studies tend to set a stroke or bleeding as an endpoint. But when you try to identify them with diagnosis names, it is difficult to determine whether it was major bleeding or stroke. A retrospective study supplements these limitations with a large population number.
In contrast, the prospective XANAP study had a continuous follow-up after patient registration. If an event occurred, the central committee evaluated it. The accuracy of the results is high because the committee decides whether to judge it as an endpoint according to certain criteria. The evaluation of the endpoint is reliable, and the probability of missing data is much lower.
The XANAP study is a real-world registry study in the Asia-Pacific region. Korean patients accounted for one third (844) of the total patients. The XANAP Korea study is a prospective real-world study that analyzed only Korean patients who took up the patient group's largest portion.
Q: What are the characteristics of Korean patients in the study?
A: They included many high-risk patients with a history of stroke. The study began in 2013 and ended in 2015. This period was before the eased NOAC’s insurance benefits. At the time, the government applied strict reimbursement standards. Only those with a history of stroke or those who have difficulty in control through warfarin were eligible for benefits.
As we recruited patients before the easing of insurance benefits, patients who previously experienced a stroke, transient ischemic attack, or central nervous system embolism accounted for about 47 percent of all patients. In other words, almost half of the patients had purposes for secondary prevention. Their mean CHA2DS2-VASc score was 3.8, a high level compared to other studies.
Q: Real-world studies can also confirm consistency with the randomized, controlled trial (RCT) that gave the basis for drug approval. Did the XANAP Korea study show consistency with the trial that supported Xarelto's approval?
A: Yes. The ROCKET-AF study, a representative RCT of Xarelto, included more high-risk patients. About 55 percent of patients had a history of stroke, systemic embolism, or transient ischemic attack (TIA). It is difficult to say that the patient group was very different. Therefore, we can say the efficacy and safety profile shown in the RCT was confirmed in real-world data.
Compared to XANTUS (a prospective real-world study in Western patients) and XANAP, XANAP Korea had a lower bleeding incidence rate, although it had more high-risk patients. Also, in both XANAP and XANAP Korea, about half of the patients had the rivaroxaban's 15mg regimen. Similarly, in real clinical settings, half of the patients receive a low-dose prescription. Nevertheless, rivaroxaban showed good results in terms of stroke or bleeding.
To balance stroke prevention and bleeding risk, physicians must prescribe the drug according to approval. However, not all conditions for each drug dosing are perfect. Doctors need a very detailed dose determination for the patient’s condition. They can adjust warfarin dose through international normalized ratio (INR) depending on patients. However, in the case of NOACs, it is difficult to fit the dosing perfectly in all patients. This is one of the unmet needs.
Apixaban and edoxaban, whose doses are reduced in half, lower the stroke prevention effect. So, doctors should be careful. On the other hand, doctors don’t reduce rivaroxaban and dabigatran dosing significantly. That is why we obtained such results. For doctors who prescribe NOACs, rivaroxaban is an easy choice to prescribe and take care of the patient’s condition.
Q: Can you share your tips for Xarelto prescription for Korean AF patients based on the XANAP Korea study results?
A: Rivaroxaban is the easiest to prescribe. There are two doses of rivaroxaban for AF patients in Korea, 20mg and 15mg. Rivaroxaban 20mg is the standard dose, but 15mg is also widely used. However, even with a low-dose prescription, the results are not bad, as real-world research showed. Japan already uses 15mg of rivaroxaban as a standard dose and chooses 10mg if renal function is poor. Taiwan recommends both 20mg and 15mg of rivaroxaban as standards, and in clinical practice, 15mg accounts for more than 90 percent of the prescriptions. In Asia, rivaroxaban 15mg is mostly used.

