Cancer patients are calling for insurance coverage of new anticancer drugs, such as AstraZeneca’s non-small cell lung cancer (NSCLC) treatment Tagrisso and Daiichi Sankyo’s metastatic breast cancer treatment Enhertu.
Both drugs have confirmed their effectiveness but have failed to overcome the high hurdle of expensive drug prices.
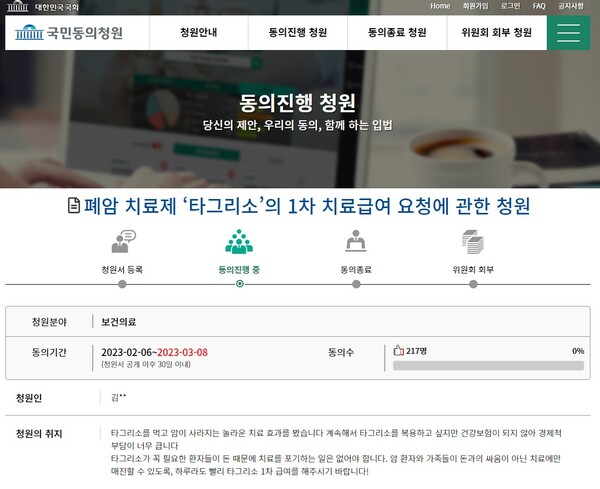
On Monday, a petition of national consent that called for providing insurance benefits for Tagrisso was sent to the National Assembly’s Health and Welfare Committee as a motion.
“After being diagnosed with stage 2 lung cancer in 2017, the surgery progress was good, but four and a half years later, it recurred in October 2021," the petitioner, who introduced himself as a lung cancer patient, said. “The MRI test showed cancer spread to the brain, and I was prescribed Tagrisso. I took the drug to clutch at straws, and my condition improved noticeably.”
About three months after taking it, he heard that all tumors were missing. The petitioner said that he is tested every three months and maintains his health by taking Tagrisso.
“Although the mass of tumor has disappeared from my body, there is a high wall of reality -- the price of medical costs,” he said.
The petitioner added that health insurance is not applied if patients use Tagrisso as the primary lung cancer treatment. Therefore, the entire medication costs come back to patients and their families.
“I have already spent more than 70 million won ($55,600) on medicine alone for more than a year. Every day is painful because of the struggle with the price of medicine," he said.
He emphasized that patients should never give up treatment because they don't have money.
“I cannot know how many patients gave up treatment due to lack of money because Tagrisso was pushed out of the list of insurance coverage. So I want Tagrisso's approval as primary treatment backed up by insurance coverage,” he said.
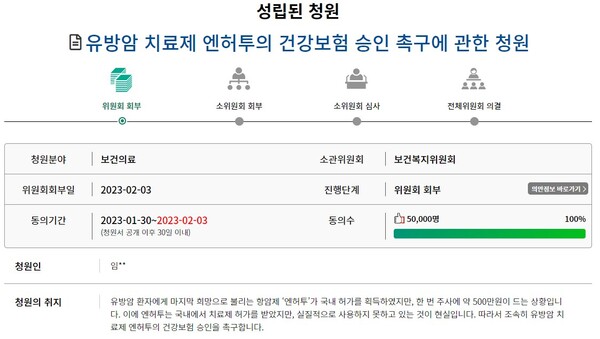
Another petition, which called for providing insurance benefits for Enhertu, was referred to the Health-Welfare Committee, garnering consent from 50,000 people. A petition is referred to the relevant committee if 50,000 people agree with it within 30 days. If adopted for the committee's review, it is tabled in the plenary session for lawmakers’ deliberation and vote.
“Enhertu, the last hope for breast cancer patients, has won domestic approval, but it takes about 5 million won for each injection,” the petitioner said. “In reality, the drug has been approved for treatment but has not been used practically. Therefore, I call for the approval of the insurance benefits for the breast cancer treatment as soon as possible."
The petitioner went on to say, “I hope Enhertu will receive insurance benefits so that many breast cancer patients, including my mother, will live their second life.”

