As the benefits of treating cancer with "radioactive" substances that emit radiation, such as alpha, beta, gamma, X-ray, and positron rays, have become established, radiopharmaceutical cancer therapy, which has been introduced for thyroid cancer, pediatric neuroblastoma, and neuroendocrine tumors, is expected to expand to prostate cancer and small cell lung cancer.
Cancer treatment with radioactive substances has been attracting attention as a next-generation cancer treatment method because it is highly effective because of its targeted treatment effect, and it has a "targeted treatment" effect while affecting non-cancerous areas less.
But there's a problem. In cancer treatment using radioactive substances, which is based on the concept of treating cancer through radiation, the treatment using radioactive substance “iodine” for “thyroid” cancer, the number one multiple cancer in Korea, and “neuroblastoma,” the most common pediatric cancer in children under the age of one, can be treated as many times as desired in Korea.
However, the treatment using the radioactive substance “lutetium” for “neuroendocrine tumor,” a rare cancer, has a regulation of six treatments, forcing patients to go abroad for treatment.
Is the reason for restricting the number of treatments in Korea the difference in effectiveness or safety between the two treatments using radioactive substances “iodine” and “lutetium”?
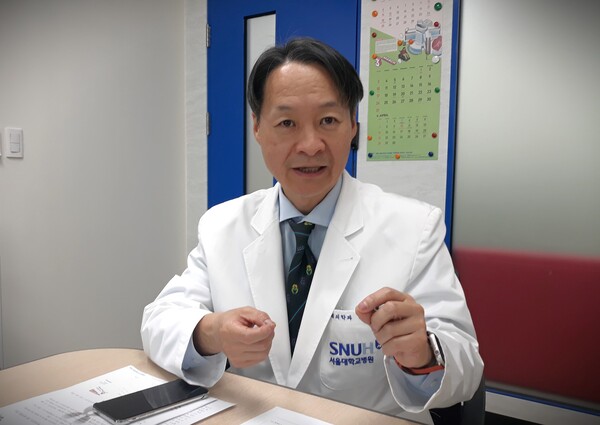
"I don't think so," said Professor Kang Keon-wook of the Department of Nuclear Medicine at Seoul National University Hospital and president of the Korean Society of Nuclear Medicine during a recent interview with Korea Biomedical Review.
"Thyroid cancer patients are treated with radioactive iodine when the cancer recurs and again if it recurs to stop the progression of the cancer in between," Professor Kang said. "Iodine treatment for thyroid cancer is almost similar to radioactive lutetium treatment for neuroendocrine tumors. Neuroendocrine tumors can be treated with lutetium just like thyroid cancer when the cancer recurs."
So why is it that only lutetium treatment has a limit on the number of treatments, forcing neuroendocrine tumor patients to receive a maximum of six lutetium treatments (four paid and two unpaid) in Korea and then travel to Germany or Malaysia for lutetium “ruthenium treatment available at home?”
This is no simple question. Many factors are involved, including Korea's unique healthcare system, which is different from other countries, the characteristics of radiopharmaceuticals, which are different from conventional anticancer drugs, and the different systems of the past and present.
However, there is hope. There is no reason why lutetium treatment for neuroendocrine tumors shouldn't be available in Korea, just like iodine treatment for thyroid cancer and neuroblastoma with an unlimited number of treatments.
Then, why have “iodine treatment” for thyroid cancer and “lutetium treatment” for neuroendocrine tumors, the two cancer treatments using not many different radioactive substances, taken different paths in Korea?
It dates back to 1998 when the Ministry of Food and Drug Safety (then the Korea Food and Drug Administration, KFDA) was established. It is responsible for the safety management system of drugs and food.
"Radioactive iodine treatment has been practiced in Germany for a long time without 'clinical trials,' and medical papers showed that it was practiced in Korea even before the establishment of the KFDA," Professor Kang said, explaining how “iodine treatment” for thyroid cancer and “lutetium treatment” for neuroendocrine tumors took different paths.
Even before the MFDS regulated treatments used on Korean patients, radioactive iodine treatment using radioactive iodine prepared by hospitals had been introduced in Korea, the number of treatments was not limited then as it is now, and there was an exception to the “approval” for treatments that had already been introduced in Korea. So, thyroid cancer and neuroblastoma patients treated with radioactive iodine are still treated freely at the discretion of their doctors.
On the other hand, radioactive lutetium, which was officially introduced in Korea in 2020, has taken a different path, even though German doctors have been using it to treat patients with neuroendocrine tumors in the same way as radioactive iodine for thyroid cancer for more than 20 years. Like radioactive iodine, radioactive lutetium has been used in Germany "without clinical trials" and formal authorization from German regulatory agencies as the counterparts of MFDS.
"Germany has a unique medical system that recognizes alternative medicine alongside modern medicine, allowing doctors to treat patients, publish research papers, and get paid if they prove some effectiveness, and both iodine and lutetium treatments were developed through this process," Kang explained.
Since its inception in Germany, radioactive lutetium therapy has spread to the Netherlands, Switzerland, Austria, Canada, Australia, Singapore, Malaysia, the Philippines, India, and Jordan. Physicians use it to treat patients with neuroendocrine tumors at their discretion, "without authorization" from regulatory agencies such as MFDS.
This means that if radioactive lutetium treatment had been introduced in Korea as a hospital-dispensed lutetium treatment at the same time as radioactive iodine treatment, the radioactive lutetium treatments could have been made without any restrictions in number.
However, regulations on the use of radioactive substances for medical purposes in Korea have been strengthened, and domestic lutetium therapy has been introduced. This treatment uses the finished radiopharmaceutical product Lutathera (lutetium oxodotreotide) instead of the radioactive isotope Lutetium.
More than a decade ago, Korean nuclear medicine doctors attempted to enact a special law on radiopharmaceuticals and manufacture the radioactive isotope lutetium in hospitals, as was the case with Germany and Malaysia but failed.
In 2017, Professor Kang had to organize a "large-scale lutetium treatment team" in Germany and Malaysia to help more than 150 patients with neuroendocrine tumors who were no longer responding to conventional treatments.
Lutathera was first introduced into Korea in November 2019 as an unapproved, urgently imported drug through the efforts of neuroendocrine tumor patients who traveled abroad with Professor Kang's help. With the government's active support, it was formally introduced in Korea in July 2020 under the Novartis' Global Lutathera Common Approval of four doses at eight-week intervals.
In other countries, the global common license for Lutathera has no problems. In Korea, however, the approval for "a total of four doses at eight-week intervals" has been interpreted as "Lutathera can be used only four times.” Is this interpretation correct, however?
"I don’t think so," Professor Kang said. "Most countries give doctors the right to treat cancer patients differently, as some people show a very high effect while others show little effect. However, Korean regulators do not recognize evidence other than that from 'clinical trials.’”
Like Korea, Lutathera is approved by regulatory agencies in the U.S., France, the U.K., and Japan for four doses at eight-week intervals. However, these countries do not limit the number of treatments to four, forcing their patients to go abroad for “expeditionary treatment.”
"Other countries use Lutathera 10 or 20 times if the effect continues and the side effects are not severe, except when resistance develops, or the side effects are severe," Kang noted. "Only Korean patients who show effects and no side effects are in a situation to stop the lutetium treatment halfway due to regulations."
Fortunately, in 2022, Professor Kang presented three medical papers from Germany, Italy, and the Netherlands as evidence to the government for the off-label use of Lutathera by the “Rules on the Standards of National Health Insurance Medical Benefits.” The rules allow patients to receive two non-reimbursed Lutathera treatments as off-label therapy in addition to the existing four reimbursed Lutathera treatments. However, there remains a big difference with other countries, which have an average of 10 to 12 lutetium treatments.
Novartis, a global pharmaceutical company, does not intend to conduct clinical trials to unlock the number of treatments for Lutathera for Korea only because the current approval is not a problem in the global Lutathera market except for Korea, and the Korean Lutathera market is not large.
A Novartis Korean official, who felt sorry for Korean neuroendocrine tumor patients being forced to undergo expeditionary treatment abroad, once emailed Novartis headquarters about the situation in Korea and asked about additional off-label clinical studies for Lutathera.
Novartis responded, "There are currently no plans for off-label clinical trials." Professor Kang's paper presented to the government in 2022 when applying for off-label use was also based on lutetium, not Lutathera.
Unlike clinical trials for other anticancer drugs, all pharmaceutical companies, including Novartis, try to keep clinical trials for radiopharmaceuticals to a "minimum" until they have proven efficacy. There's a reason for this.
"Unlike other anticancer drugs, including antibody therapies or immune checkpoint inhibitors, radiopharmaceuticals are expensive to produce and require high transportation costs due to the isotope's short half-life. Other anticancer drugs are cheaper than radiopharmaceuticals, so clinical studies continue until they fail. Still, radiopharmaceuticals cost about 10 million won ($7,390) in material costs, including transportation costs, for a single treatment. So, clinical trials are conducted with 'minimal treatment' to show the drug's effectiveness," Kang explained.
He emphasized that the four treatments of Lutathera do not mean “up to four treatments are safe,” but “at least four treatments are needed to see the therapeutic effect of Lutathera.”
"Two treatments are ineffective, and four treatments are required to prove the effectiveness of Lutathera before it can be approved, so the pharmaceutical company has done the minimum clinical trials," Kang said. “In other countries, doctors can treat 10 or 20 times on their own, but in Korea, the government controls even non-reimbursed cancer treatment, making patients suffer."
The problem of regulating the number of radiopharmaceutical treatments that use radioactive substances to stop cancer from progressing is not expected to end with neuroendocrine tumor patients. This is because all new radiopharmaceutical drugs for various cancers, such as small cell lung cancer, including Novartis' prostate cancer radiopharmaceutical Pluvicto, which will be introduced in Korea, are bound to face the same problems as Lutathera for neuroendocrine tumors due to the unique systemic issues in Korea.
"Korea is the only country that limits the number of treatments with an approval requirement for radiopharmaceuticals," Professor Kang said. "It is a system that does not meet global standards, and this problem extends to all radiopharmaceuticals for all cancers that will be introduced in the future. So the same problem is bound to occur in other cancers in the future. It is right for the Ministry of Health and Welfare to take the lead to solve the problem."
Related articles
- Government considers expanding treatment options for Korean neuroendocrine tumor patients
- Restriction on Lutathera treating neuroendocrine tumors eased this month
- SK biopharmaceuticals acquires radiopharmaceutical drug candidate from Full-Life Technologies through licensing deal
- Radiofrequency ablation of thyroid nodules effective and safe: 10-year study

