The Somzz app, Korea's first digital therapy device for mobile cognitive behavioral therapy for insomnia (MCBTi), has been proven effective in treating chronic insomnia.
A Korean study has found that MCBTi based on the Somzz app, which provides real-time personalized feedback, was effective in treating chronic insomnia by improving insomnia severity, sleep efficiency, wakefulness, sleep satisfaction, depressive symptoms, and quality of life.
Seoul National University Hospital (SNUH) said Tuesday that a collaborative research team has confirmed it after dividing 98 adult chronic insomnia patients recruited from three hospitals into two groups -- a group using the Somzz app (49 patients) and a control group using a simple sleep habit education app (49 patients) -- treating them for six weeks and following them up for four months.
Professor Lee Yu-jin of the Department of Psychiatry at Seoul National University Hospital, Professor Kim Seog-ju of the Department of Psychiatry at Samsung Medical Center, and Professor Lee Heon-Jeong of the Department of Psychiatry at Korea University Anam Hospital collaborated on the study.

Insomnia is a common sleep disorder with a prevalence of about 10 percent in the general population. Its treatment is important because of its negative impact on physical and mental health. Cognitive behavioral therapy for insomnia (CBTi) is the first-line treatment for chronic insomnia. Still, access is limited due to the time constraints of face-to-face therapy and a lack of trained professionals. Mobile app-based CBTi (MCBTi) has been developed to solve this problem, making it easier to treat more patients.
Until now, few studies have evaluated the effectiveness of mobile app-based cognitive behavioral therapy, and few have been rigorously validated using a multicenter, single-blind, randomized controlled trial.
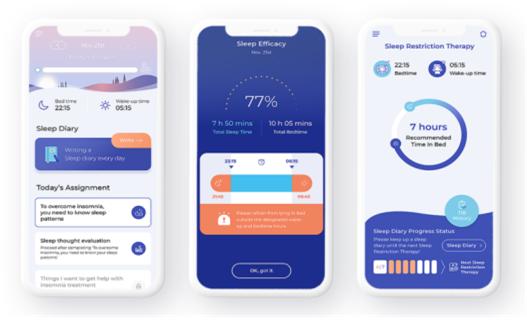
In this study, the Somzz group received real-time feedback on their sleep behavior and a sleep restriction regimen that allowed them to set customized bed and wake times, stimulus control therapy, relaxation therapy, sleep habits education, and relapse prevention education. The control group received basic sleep education through sleep hygiene education and audio-visual materials and was encouraged to keep a daily sleep diary.
The study's primary endpoint was the Insomnia Severity Index (ISI), and secondary endpoints included sleep diaries and mental health self-report questionnaires.
The results showed that the Somzz group had significantly lower ISI scores at the end of treatment and three-month follow-up. The post-intervention ISI score of 9.0 was significantly lower than the control group's 12.8. At the three-month follow-up, the ISI score for the intervention group was 11.3, lower than the 14.7 score for the control group, confirming that the treatment effect was sustained.
That showed cognitive behavioral therapy for insomnia with the Somzz app is more effective in reducing the severity of insomnia, the researchers explained. In particular, the post-treatment insomnia remission rate (ISI score of less than 8) was 45 percent and the treatment response rate (ISI score drop of more than seven points) was 57 percent in the Somsz group, proving effective in improving insomnia outcomes and reducing symptoms.
In addition, sleep efficiency (SE), the ratio of total sleep time divided by time in bed, was 78.3 percent in the treatment group, compared to 70.6 percent in the control group. The time awake after sleep onset (WASO), a measure of time spent awake, was 53.0 minutes in the treatment group, compared to 65.3 minutes in the control group.
Mental health metrics also favored the Somzz users. The depression score (PHQ-9) was 6.6 in the Somzz group, compared to 8.7 in the control group. Quality of life scores (SF-36) were 72.4 in the Somzz group compared to 63.5 in the control group.
The dropout rate was 12.2 percent (six patients out of 49) in the Somzz group. The researchers noted that it was lower than the dropout rate of in-person cognitive behavioral therapy for insomnia (up to 40 percent), indicating high adherence to a non-face-to-face digital treatment device like Somzz.
“This study shows that cognitive behavioral therapy with Somzz, the first digital therapy device in Korea, is highly effective in treating insomnia,” Professor Lee Yu-jin said. “In particular, the significant improvements in insomnia severity, sleep efficiency, wake-up time, sleep satisfaction, and mental health suggest that Somzz can be used as an efficient and accessible treatment for insomnia.”

