The earliest and tiniest preemies (twins) born in Korea recently returned home to their families.
The twins, who came into the world at 22 weeks and three days weighing just 410 grams, could leave the hospital weighing 4 kilograms, nearly 10 times heavier than when they were born. Their chances of survival were zero percent, but the dedication of the medical staff at Chungnam National University Sejong Hospital and the love of their parents created a miracle.
According to the International Classification of Diseases, the survival perinatal period is defined as 22 weeks of gestation, but the actual chances of survival become meaningful when the baby weighs at least 500 grams.
The actual chances of survival for premature babies less than 24 weeks of gestation are only around 20 percent, and the chances of survival for twins are so slim that there are no statistics. The hospital has set a new milestone in treating extremely low birth-weight twins in Korea.
Moreover, it is difficult to find a hospital willing to accept mothers who have just passed 22 weeks of pregnancy and treat premature babies in rural areas “that are dwindling fast.” On March 4, a mother of twins whose water suddenly broke in her fifth month of pregnancy was transferred from Daejeon, where she lived, to Sejong. It was right after trainee doctors began to resign en masse in protest of the government's push to increase the number of medical students, aggravating the situation.
Chungnam National University Sejong Hospital accepted the mother only for the single purpose of “saving the mother and fetuses.” A miracle was born, but initial chances of survival were challenging to estimate.
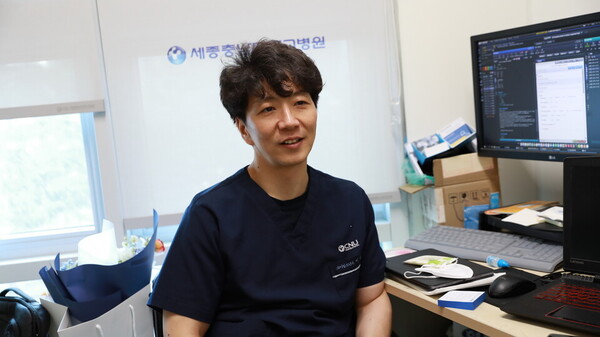
“Every day was a struggle,” recalls Professor Lee Byung-kook, head of the NICU at the hospital, who has been treating the twins since their birth. The twins were in the NICU, with medical staff by their side around the clock. Professor Lee’s wife, a nurse, ordered her husband “not to come home until they're alive,” helping him focus on the twins.
The twin brothers, who were intubated and otherwise resuscitated immediately after birth, were barely breathing on a ventilator until they were 50 days old. The elder brother had to undergo surgery for a perforated intestine caused by necrotizing enterocolitis at 40 days old. He endured a trip to Seoul to treat retinopathy of prematurity just after 100 days. The second had a pneumothorax at two days old. They underwent a procedure to insert a chest tube into his tiny chest. The goal was to “keep him alive without complications.”
“We are running the NICU with the idea that small children (like the twins) should be accepted even if there is no place for them because if we don't accept them, who will? I wasn't confident I could save them, but I am trying my best today. We can only wait for the outcome, and I greatly desire to move forward so that they can get better without complications,” Lee said during a recent interview with Korea Biomedical Review.

Despite his modest answer, Lee is a skilled doctor who has saved the fourth smallest baby in Korea, weighing 370 grams. Last year, he also attained a 100 percent survival rate for premature babies born at 23 weeks or more.
However, Professor Lee emphasized that it was the sacrifices of numerous medical workers from “beyond the region” that made it possible for him to protect critically ill newborns that many in the region shun. The first retinopathy of prematurity surgery was performed by a professor at Seoul National University Hospital, and the second was performed by a pediatric surgeon at Chungnam National University Hospital.
“In neonatal medicine, problems in every part of the body need to be treated. When the baby had retinopathy of prematurity, the ophthalmology department took care of it, and when he needed surgery, a pediatric surgeon from Chungnam National University Hospital traveled to perform the surgery. For pediatric skin problems, the dermatology department also consulted,” Lee said.
It's not just the medical staff. Professor Lee also shared an anecdote about how he was touched by a cleaning lady who was cleaning the NICU a few days ago. “As I was mopping the NICU, I thought to myself, 'I have to keep it clean so that the children can live,' and I realized that so many people in the hospital are trying to keep the children alive,” he said. I realized that so many people are pouring out their “blood, sweat, and tears” for the “well-being” of children in the NICU.
However, the reality is that hospitals have to bear the burden of “financial loss” after treating extremely low birth weight babies.
Many medical workers are willing to pour out their “blood, sweat, and tears” to save lives, but it is only the result of “grinding human labor into it.” Even though there are five doctors, including Professor. Lee, guarding the NICU, Lee still spends 140 hours of his 168-hour workweek at the hospital. The hospital cannot make the necessary investments to advance neonatal intensive care medicine in a system where the more you treat, the more you lose. The rural situation is even worse.
“The government has introduced fees to incentivize doctors to visit provincial hospitals. However, it's useless if the money doesn't go to the doctors because they have no reason to stay in the regions,” Lee said.
Professor Lee pointed out that the health system is one of the social systems in Korea that is supposed to equalize the regions. It's concentrated in the metropolitan areas because people are not incentivized to stay in the regions.
“Physicians want to live in places with the infrastructure to live with their family. To keep them in regions by sacrificing that desire, the society should provide corresponding incentives,” Lee added.
Related articles
- Miracle twins: premature babies born at 22-week, 400 grams defy odds
- Why do Korean mothers give birth to twins mainly through C-sections?
- Triplets born at 22 weeks discharged healthy after intensive NICU treatment in Seoul
- Korea still relies on manual jobs to provide nutrition therapy for preterm infants: experts

