A condition has received better treatment in recent years as more therapies have been covered by health insurance. It is a severe atopic dermatitis.
Atopic dermatitis is a chronic inflammatory skin disease caused by genetic and environmental factors.
Since Sanofi's Dupixent (dupilumab) got insurance benefits in 2020, several treatments have followed its example. They include AbbVie's Rinvoq (upadacitinib), Lilly's Olumiant (baricitinib), Pfizer's Cibinqo (abricitinib), and Leo Pharma's Adtralzar (tralokinumab), expanding the number of drug options.
However, while it's encouraging to have more options for treating severe atopic dermatitis, healthcare providers and patients alike are concerned that switching between medications is not covered by health insurance, leading to a lack of personalized care. Even if the first medication is ineffective or has side effects, switching medications is not covered by health insurance, so not many people switch to another medication.
To be eligible for reimbursement for switching to a different drug, patients must have been on the first-line treatment for three months and meet the criteria of an Eczema Area and Severity Index (EASI) of 23 or higher. Otherwise, they must pay out-of-pocket for up to 17 million won ($12,770) of medications annually. Allowing patients to switch medications is a way to increase patient choice and save health insurance funds.
On Saturday next week, the Severe Atopic Dermatitis Association, a group of severe atopic dermatitis patients, and Rep. Jeon Jin-sook of the Democratic Party of Korea will co-host a policy discussion sponsored by the Korean Atopic Dermatitis Association on “How to Improve the Treatment Environment for Severe Atopic Dermatitis. "
The policy debate, which celebrates World Atopic Dermatitis Day on Sept. 14, will feature discussions between the association, patients with severe atopic dermatitis, and Rep. Jeon on how to improve the treatment environment for severe atopic dermatitis, which is limited by unreasonable reimbursement standards.
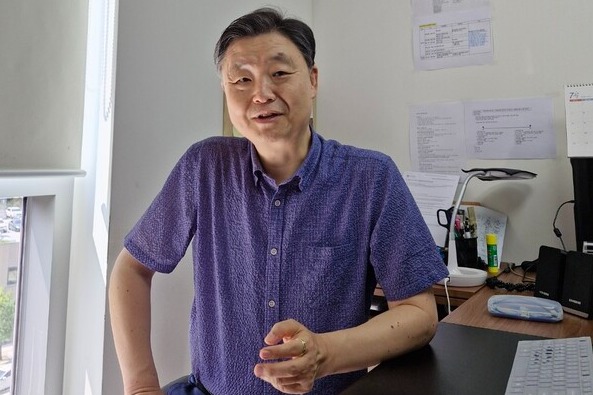
Before the event, Korea Biomedical Review met with Dr. Choi Eung-ho, president of the Korean Atopic Dermatitis Association and a professor of the Dermatology Department at Wonju Severance Christian Hospital, to learn about the need to allow switch dosing.

Question: Severe atopic dermatitis treatments have been rapidly receiving insurance benefits in recent months. The treatment landscape for severe atopy seems to have improved in recent years.
Answer: The treatment environment for severe atopy is changing rapidly. In the past, quite a few patients couldn't afford it, but nowadays, even expensive drugs are covered by health insurance. Moreover, most of the new drugs that have been in clinical trials overseas are now covered. The patient's burden is only 10 percent because they can apply the calculation special exception system. I heard that Korea is among the countries that use the most expensive severe atopy drugs concerning the population because of the particular exemption system.
The problem is that despite good treatment conditions, such as the introduction of new drugs, health insurance coverage, and the reimbursement system, there are still limitations in choosing the proper treatment for patients. Switching between biologics and JAK inhibitors, and even between drugs in the same class, is not reimbursed. Choosing the proper treatment for a patient requires a trial of multiple agents, which is not always possible in severe atopic dermatitis. It's not that you can't try other drugs, but you have to forgo health insurance coverage and pay for them. How many patients can afford to do this for the rest of their lives?
Q: There are many difficulties in choosing a treatment since switching is blocked.
A: Depending on the patient's symptoms and financial situation, Dupixent is the most commonly prescribed. It's the oldest and most prescribed drug, so we can't ignore its clinically proven effectiveness. However, some patients are less effective than expected or suffer from side effects. If doctors say, “Let's try switching to another drug, but to be covered by health insurance, we have to go back to the beginning and use first-line drugs such as cyclosporine and methotrexate for three months,” most patients reply, “It's not perfect, but we can't go back.”
If doctors have patients who say, “This is the happiest time of my life,” they cannot reply, “We can't afford it; let's switch to a different drug because it is less effective and has side effects.” In the end, you're stuck with the most expensive drug, Dupixent, even if it doesn't work and has side effects. This is a clear loss for health insurance finances.
Q: To what extent do you think allowing switch dosing will affect health insurance finances?
A: We have done our financial impact analysis. The annual health insurance expenditure for severe atopic dermatitis was estimated to be 43 billion won. Still, it would decrease to 25 billion won if substitution was allowed. A 42 percent annual savings of 18 billion won is expected even at a cursory calculation. Of course, the substitution rate is only a prediction based on overseas papers, so there may be disagreements. However, allowing substitution will undoubtedly save health insurance funds.
Q: Are there any problems with allowing switch dosing?
A: Switching between drugs is allowed in rheumatologic diseases, where biologics are used. This is even though rheumatologic patients are much older and, therefore, more likely to experience adverse events. The reality is that we allow people with a high risk of adverse events and do not allow switching in severe atopy, where the average age is 30.
Q: Is there a biomarker for atopy that can tell patients which medications will work for them?
A: There are no biomarkers for severe atopic dermatitis yet. However, as we accumulate more data on atopic patients, the probability of what works for some people will increase so that AI can be introduced to atopic treatment. Europe introduced precision medicine three to four years ago. AI learns to prioritize which medication to administer by inputting patient information. This is only possible if you have much information about the patient, so switching medications should be allowed.
Q: Lastly, when we look at atopic dermatitis patients, we think there are still a lot of people who miss the timing of treatment because they are still using herbal or folk remedies.
A: Korea is not a scientific society. With the new government marginalizing science in national policy, I wondered if Korea has no intention of becoming an advanced country or a leader. The inability to think scientifically leads people to seek folk remedies or oriental medicine. Non-scientific methods have taken over because they have not been able to provide a precise treatment method. However, the treatment environment has changed recently. In that regard, I think it will be a thing of the past to see atopic dermatitis patients in oriental clinics in two to three years.
Related articles
- Dermatologists call for personalized treatment, subjective symptom focus for eczema
- Lilly Korea’s new atopic dermatitis drug ‘Ebglyss' receives approval
- Sanofi’s atopic dermatitis drug Dupixent gets expanded coverage for treating children under 5
- Kangstem Biotech’s shares plummet after phase 3 atopic dermatitis study fails
- Dermatologists call for insurance coverage expansion for atopic dermatitis treatments
- Calls mount for cross-dosing of atopic dermatitis treatments to alleviate insurance burdens as Dupixent dominates market
- Misconceptions, treatment strategies addressed for atopic dermatitis in health talk show
- Disallowing cross-dosing of severe atopic dermatitis drugs comes under parliamentary scrutiny
- ‘Dupixent is cost-effective drug for asthma, which requires ₩4 trillion yearly’
- Patient group, Danish Embassy call for allowing cross-dosing of drugs to treat severe atopic dermatitis
- ‘Placenta shots are effective in treating atopic dermatitis’
- ‘Adtralza with adjustable dosing intervals increases satisfaction of people with atopic dermatitis’
- Expanded reimbursement for Rinvoq enhances atopic dermatitis treatment options
- Sanofi Korea wins approval to expand Dupixent indication for certain COPD patients
- AbbVie’s Rinvoq expands reimbursement in Korea for psoriatic arthritis

