Recent guidelines in Korea for high-risk atherosclerotic cardiovascular disease (ASCVD) patients have shifted, recommending a substantial reduction in low-density lipoprotein cholesterol (LDL-C) levels from 70 mg/dL to below 55 mg/dL—an ambitious target that reflects the growing consensus that "the lower, the better" for heart disease prevention.
But even with the most advanced statin therapies, many patients are still falling short.
“Despite high doses of oral treatments, one-third of patients can’t reach the LDL-C target of 70 ( mg/dL),” said Professor Kim Byeong-keuk of cardiology at Severance Hospital. “With the new target of 55 ( mg/dL), more than 40 percent could still miss the mark.”
Professor Kim spoke at an open campus program hosted by Novartis Korea on Thursday, where he offered an overview of Leqvio (ingredient: inclisiran), a first-in-class small interfering RNA (siRNA) treatment that gained regulatory approval in Korea this past June.

However, Kim stated that the issue of achieving LDL-C targets isn't just about the drugs; it's about patient adherence.
“When patients stick to their treatment plans, their outcomes improve dramatically,” Kim explained. “But as regimens become more complicated, adherence falls off. Multiple medications, large pills, and frequent doses all contribute to patients abandoning their treatments.”
Adherence isn’t just a nice-to-have; it’s a necessity—especially for older patients battling atherosclerosis. Polypharmacy is a growing issue, and as treatment intensifies, so does the challenge of getting patients to stick with it, particularly the elderly, who face additional hurdles in remembering their medications.
In Korea, the problem is compounded by a rising number of single-person households, where older adult patients are often left to manage their treatment alone. "Even with reminders and nurse consultations, compliance remains stubbornly low," Kim noted.
For chronic conditions that involve multiple risk factors, achieving full control is even harder. According to Kim, that’s why improving adherence is just as critical as developing new medications. “The fewer times patients have to take their medication, the better,” he said.
Unlike oral medications, which require frequent doses, Leqvio offers a far simpler regimen—just two injections in the first year, then one every six months after that. For patients, this means near-perfect compliance. "It’s essentially a guaranteed compliance rate," Kim said. "We’re not just prescribing a drug; we’re delivering a treatment that healthcare providers can ensure was given as intended."
In a world where even a two-week regimen is prone to missed doses, Kim said Leqvio's biannual injections could be a potential game-changer. When compared to the more frequent dosing required by anti-PCSK9 monoclonal antibodies (mAbs), siRNAs like Leqvio offer a much more favorable adherence profile. "An injection every six months offers almost perfect adherence," Kim said.
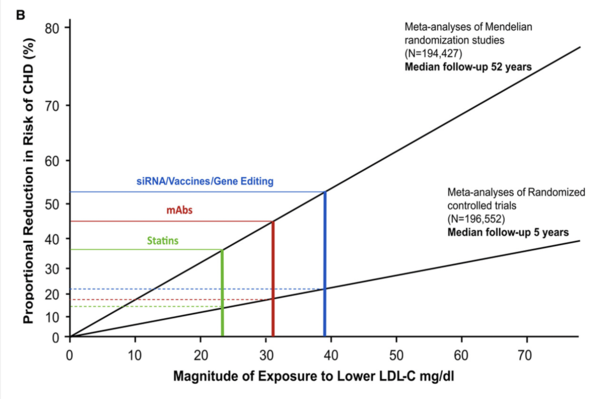
In Korea, where these treatments are administered directly in healthcare settings, Kim believes adherence could "realistically reach 100 percent." This, he argued, isn't just a minor improvement—it's a significant shift in how we approach cardiovascular care. "It's essentially a new treatment strategy," he said.
The phase 3 ORION clinical trials—ORION-9, ORION-10, and ORION-11—showed that Leqvio significantly reduced LDL-C levels in patients with ASCVD or equivalent risk, and heterozygous familial hypercholesterolemia (HeFH). By Day 510, Leqvio reduced LDL-C by 47.9 percent, 52.3 percent, and 49.9 percent in treatment groups compared to placebo (P<0.001).
The more recent ORION-18 trial, conducted with Asian collaborators including Korea, showed similar results. Participants received an injection every three months initially, followed by one every six months. 57.2 percent of participants experienced steady LDL-C reduction, with some exceeding 60 mg/dL. Follow-up results showed that the 50 percent reduction in LDL-C persisted for up to six years, even in those who resumed treatment after a placebo period.
For countries like Korea, where insurance typically covers biannual treatments, Kim emphasized that Leqvio represents an ideal solution. "Over 80 percent of patients who come for outpatient visits only need to come twice a year," Kim noted.
However, despite the promising results, Korea’s insurance coverage for Leqvio is lagging behind. "We haven’t even started discussions on insurance coverage," Kim said. "It’s disappointing, especially since this isn’t just about the drug itself. This treatment could define the future of cardiovascular care."
Related articles
- Korea becomes a battlefield for multinational drugmakers developing ASCVD drugs
- Novartis’ twice-yearly dyslipidemia drug wins approval in Korea
- Novartis’ Entresto reduces mortality and hospitalization risks in Korean patients, PARADE-HF study shows
- Novartis' lipid-lowering drug Leqvio clears reimbursement hurdle on 1st attempt

