A Korean study has confirmed that lowering systolic blood pressure below 140 mm Hg immediately after endovascular recanalization treatment in patients with acute cerebral infarction has a negative impact on their prognosis.
The Patient-Centered Clinical Research Coordinating Center (PACEN) under the National Evidence-based Healthcare Collaborating Agency (NECA) said so on Friday, releasing the results of a clinical value assessment of the study “Comparison of blood pressure management strategies after endarterectomy in patients with acute cerebral infarction.”
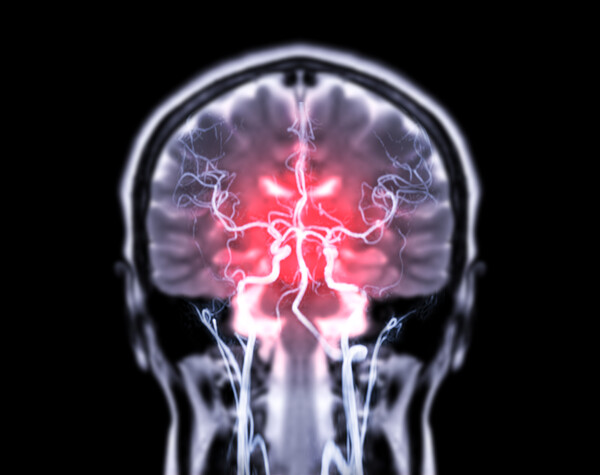
Cerebrovascular disease is the leading cause of death in Korea. Due to the nature of stroke, even if acute-phase treatment is successful, it is a burdensome disease not only for the individual patients but also for the society and economy due to sequelae, including motor and speech disorders.
The study result came amid the recent increase in the use of intra-arterial thrombectomy as a treatment for recanalization of acute cerebral infarction, causing controversy over the goal of blood pressure control during the first 24 hours after intra-arterial thrombectomy, a high-risk period for several vascular events, including cerebral hemorrhage and progression of cerebral infarction.
Korean and foreign guidelines recommend lowering blood pressure to 180/105 mm Hg or lower for 24 hours after endarterectomy.
However, no high-quality prospective comparative clinical studies have been conducted to support this recommendation, and related retrospective studies have reported conflicting results.
Against this backdrop, the PACEN supported the OPTIMAL-BP study, conducted by Professor Nam Hyo-suk and colleagues at Yonsei University, to compare blood pressure control treatment strategies in patients with acute cerebral infarction immediately after successful endovascular recanalization to optimize patient health outcomes.
The OPTIMAL-BP study was a randomized, comparative clinical trial conducted at 19 medical institutions in Korea from June 2020 to November 2022.
The results showed that patients in the group that had their systolic blood pressure lowered to less than 140 mm Hg immediately after endovascular recanalization therapy had a 15.1 percent larger share of patients with a poorer prognosis compared to those in the standard blood pressure management group of 140 to 180 mm Hg.
Researchers said the findings will likely inform evidence-based treatment strategies in clinical practice and future guidelines, which specifically state that systolic blood pressure should be maintained below 180 mm Hg for 24 hours after endarterectomy in patients with acute cerebral infarction but should not be overly controlled below 140 mm Hg.
According to PACEN, the study subject is one of the most under-researched areas because no specific entity directly benefits from the research.
The study was published in the Journal of the American Medical Association (JAMA), one of the world's most prestigious medical journals, and was recognized as an excellent example of research that confirms that public support for clinical research can bring real benefits to the public's health.
“These findings can be used as an important basis for selecting treatment strategies in clinical practice and are an excellent example of improving the awareness of clinical trials among Korean patients,” said Dr. Heo Dae-seog, director of PACEN.
Patient-centered, state-supported public-interest clinical research can bring real health benefits by supporting research that identifies what is best for patients, and state support for public-interest clinical research must continue, Heo added.

