Aseptic dissociation, a loosening of the fixation between the artificial joint and the bone, has been identified as the leading cause of reoperation in patients following hip surgery.
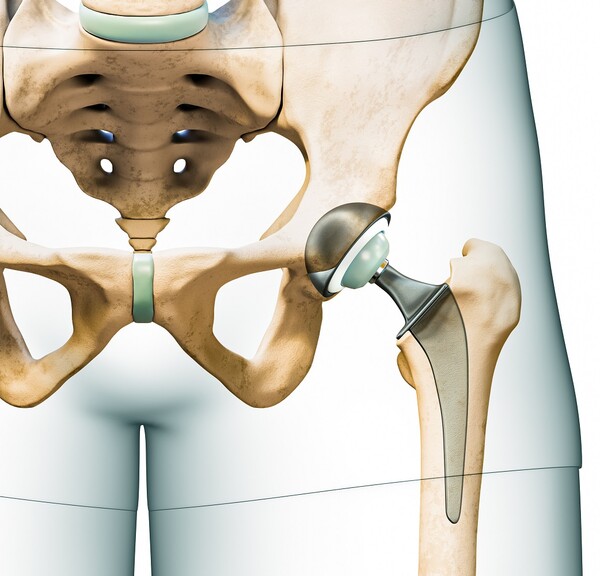
Hip surgery is a procedure that replaces the hip acetabulum and femoral head with an artificial implant to reduce pain and restore function. It is a treatment for degenerative arthritis and femoral head necrosis of the hip joint. While most patients return to normal activities, some will require revision surgery over time.
Because revision hip surgery is more complex and has a poorer prognosis than the initial procedure, placing a greater physical and mental burden on patients, it is essential to accurately identify and manage its causes.
However, it has been difficult to accurately identify the factors that cause revision surgery because they can vary depending on the time since surgery.
A team led by Professors Lee Young-kyun and Park Jung-wee of the Department of Orthopedic Surgery at Seoul National University Bundang Hospital (SNUBH) said Tuesday that they comprehensively analyzed the causes, timing of occurrence, changes in surgical techniques and fixation methods for all 515 artificial hip revision surgeries performed at the hospital from 2004 to 2023, and divided the timeline into two phases -- 2004 to 2013 and 2014 to 2023 -- reflecting major advancements in surgical techniques and implant materials after 2013.

The study found that the most common cause of all hip revision cases was aseptic dissociation (52.4 percent), a loosening of the fixation between the artificial joint and bone without infection, resulting in a weak and unstable bond. This was followed by infection (13.2 percent), periprosthetic fracture (10.7 percent), wear and osteolysis of the prosthesis (8.5 percent), ceramic breakage (5.8 percent), and dislocation and joint instability (5.6 percent).
The proportion of these reoperation causes varied significantly by the time of surgery. Aseptic dissociation accounted for 62.5 percent in stage 1. Still, it decreased significantly to 40.4 percent in stage 2, which the researchers attributed to improved insert materials and advances in surgical techniques that reduced wear and fixation failure.
On the other hand, the rates of infection, periprosthetic fracture, wear and osteolysis of the prosthesis, and ceramic breakage tended to increase in the second-stage surgery group.
The leading causes of reoperation also differed depending on the time since hip surgery. Within the first few years after surgery, complications, such as dislocation, periprosthetic fracture, and infection, were the leading causes, while more than 10 years after surgery, aseptic dissociation, wear and tear of the prosthesis, and osteolysis were the leading causes.
“These findings suggest that the risk factors to watch out for and manage change over time after artificial hip surgery,” Professor Lee said. “If utilized, it may be possible to develop a systematic postoperative management plan to prevent reoperation.”
Professor Park said, “Advances in surgical materials and methods have reduced the proportion of reoperations related to wear and tear on the articular surface, but dislocation and infection around the prosthesis are still major causes. We will continue our research to find ways to reduce the number of reoperations.”
Related articles
- Korean professor becomes 1st to win ATS award for lung cancer research
- SNUBH study finds colon cancer patients regain quality of life within 7 weeks after laparoscopic surgery
- SNUBH study finds lymph node dissection unnecessary in some endometrial cancer cases
- Alcohol misuse and mental illness share genetic roots, study finds

