An international consensus statement outlining antiplatelet treatment strategies for East Asians has recently been released.
For the first time, treatment principles that take into account the unique bleeding risks and antiplatelet responsiveness of East Asians have been articulated, marking an important milestone in the transition to precision medicine in cardiovascular care in the region.
Recently published in the July issue of JACC: Asia, the American College of Cardiology's journal, the “Position Statement on Antiplatelet Therapy for East Asians With Coronary Artery Disease” is the first multinational recommendation developed by cardiology leaders from more than 10 East Asian countries, including Korea, China, Taiwan, and Singapore.
“This consensus statement was developed in collaboration with the Chinese Society of Cardiology and is a significant step forward in advancing the concept of precision medicine based on the ‘East Asian Paradox’ that we have been developing,” said Professor Jeoung Young-hoon of the Department of Cardiology at Chung-Ang University Gwang Myeong Hospital and former Vice President of the Asian Society of Cardiology. “We hope this publication will make an important contribution to personalized antiplatelet therapy for East Asians.”
Unique bleeding-ischemia balance in East Asians requires accurate risk assessment
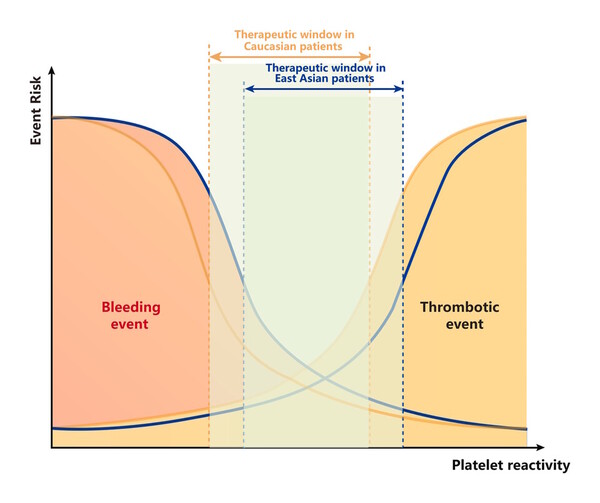
The “East Asian Paradox” was first suggested in 2012. It stems from the observation that East Asian patients have a lower risk of cardiovascular events than Westerners, but a higher risk of bleeding when using antiplatelet drugs.
It is explained by a multifaceted interplay of biological factors beyond simple ethnic differences, including genetic factors (e.g., CYP2C19 metabolism gene variants), lower body weight, susceptibility to gastrointestinal bleeding, and lower inflammatory and coagulation activity.
The consensus statement notes that “the risk of bleeding is very high in East Asians, whereas the risk of ischemia is relatively low, and therefore the same benefits cannot be expected from high-intensity antiplatelet therapy as in the West,” emphasizing that quantitative assessment of bleeding-ischemia risk from the outset and adjusting treatment intensity and duration accordingly is key.
The consensus statement points out that potent P2Y12 inhibitors (ticagrelor, prasugrel), currently considered the Western standard, may increase the risk of bleeding in East Asians, with similar or worse ischemia prevention.
For example, in large trials such as TALOS-AMI, TICA-KOREA, and PHILO in Korea and Japan, ticagrelor was associated with up to twice the incidence of major bleeding compared to clopidogrel; however, it did not show a significant difference in ischemic prevention.
The consensus statement therefore proposed a strategy of “de-escalation” to clopidogrel at an early point (within one month) as the default, even in patients requiring initial high-intensity therapy. It also recommended a short course of clopidogrel-based dual antiplatelet therapy (DAPT) before switching to single-agent therapy in patients at high bleeding risk (HBR).
The consensus statement points out that the existing Western-based high bleeding risk (HBR) assessment tool, ARC-HBR, does not reflect the reality of East Asian patients, and introduces East Asian-specific assessment tools (J-HBR, KAMIR-DAPT, and others) developed by the Korea Acute Myocardial Infarction Registry (KAMIR) study conducted by the Japanese Cardiology Society (JCS) and the Korean Society of Cardiology.
For example, the J-HBR criteria categorize underweight as a significant risk factor, “55 kg or less for men and 50 kg or less for women,” which is often overlooked in Western criteria. In practice, it has been reported that the risk of high bleeding among East Asian patients is as high as 60 percent when using these criteria.
The consensus statement specifically emphasized the strategies of “shorter DAPT duration” and "early single-agent switching. Many recently published trials (STOPDAPT-2, HOST-IDEA, and T-PASS) from Korea, Japan, and elsewhere have shown that switching to clopidogrel monotherapy after a short DAPT of one to three months in East Asian patients maintains ischemia protection and significantly reduces bleeding risk.
While this strategy is still considered conservative by Western guidelines, the consensus statement states that it can be considered the “default strategy” in East Asia.
Future challenges: standardizing risk scores and establishing diagnostic algorithms
However, the consensus statement also noted that an integrated risk scoring system for bleeding and ischemia, which can be used across East Asia, is still lacking. Currently, scoring systems have been developed in Japan, China, and Korea; however, they lack unified guidelines and long-term follow-up studies.
As a result, they plan to develop a risk score that can be used jointly across East Asia and standardize guidelines for use across the region.
According to experts, the consensus statement is more than just a clinical guideline; it is a global formalization of the “personalized treatment principle” that reflects the biological characteristics and medical realities of East Asian patients.
"The concept of the ‘East Asian paradox’ is not just an observation but should now become a core paradigm for designing treatment strategies," Professor Jeong said. "We hope that this consensus statement will serve as the evidence base for Korean antiplatelet therapy."

