Korean researchers have found that biportal endoscopic discectomy (BED), a surgical procedure for lumbar disc herniation (commonly known as a herniated disc), offers functional outcomes comparable to conventional surgery while providing greater safety and better recovery. Studies have shown that while the clinical outcomes of BED are equivalent to those of conventional surgery, it results in less pain, scarring, and fewer complications.
A herniated disc is a condition in which a disc in the lumbar spine ruptures and the leaking nucleus pulposus compresses the nerves, causing back pain, sciatica (pain radiating from the buttocks to the legs), and leg tingling. Most cases can be treated with medication or physical therapy. However, if the condition is accompanied by loss of muscle strength, difficulty with bowel movements, and persistent pain, surgery is required to remove the leaking nucleus pulposus.
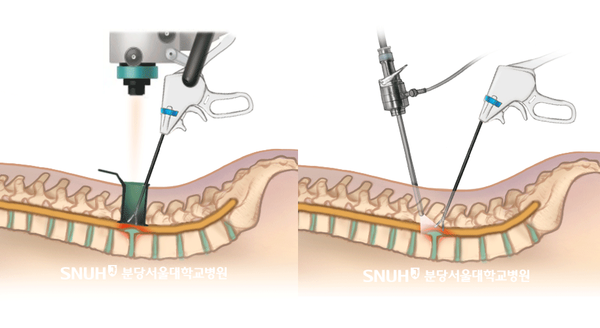
The current standard of care is a microscopic discectomy (MD), which involves making a 30~40mm incision in the muscles of the lumbar spine and removing the leaking nucleus pulposus under a surgical microscope. It is faster to recover and less painful than the previous open surgery method. Still, it has limitations in that damage, scarring, and pain are inevitable during the process of spreading the muscles.

Seoul National University Bundang Hospital (SNUBH) said Monday that a team led by Professor Park Sang-min of the Department of Orthopedic Surgery randomly assigned 100 patients who underwent surgery for lumbar disc herniation at six hospitals in Korea from July 2021 to September 2022 to 50 patients each in the BED and MD groups, and followed the patients for 12 months after surgery.
BED is a surgical method that removes the nucleus pulposus by making only about 10mm to 20mm incisions in two lumbar vertebrae and checking the area with an endoscopic camera, while MD is a surgical method that requires a larger incision than bilateral endoscopic discectomy because the area must be viewed under a microscope. The study examined functional recovery scores, early recovery indicators (pain, muscle damage, scarring, and others), and complications according to these differences in surgical methods.
The results showed that there was no significant difference in functional recovery scores between BED and MD. The mean functional recovery scores at 12 months postoperatively were statistically similar at 10.92 and 10.38, respectively. This suggests that BED is as effective at removing the nucleus pulposus as MD.
On the other hand, BED performed better on early recovery metrics. Surgical site pain was lower in the BED group at both 24 and 48 hours postoperatively, and muscle damage was also significantly lower in the BED group. Scar scores were also better in the BED group at three and six months. This was related to the incision length, which averaged 15.8 mm in the BED group, less than half the average of 33.1 mm in the MD group.
Complication rates also favored the BED group, with zero cases of wound dehiscence in the BED group and five cases in the MD group. Other than that, reoperations and serious adverse events (such as cardiovascular death) were not seen in either group.
“This study is significant because it is the first to demonstrate that bilateral endoscopic discectomy is clinically superior in terms of scarring, early pain, and muscle damage, with similar functional recovery outcomes to conventional surgery,” Professor Park said. “Endoscopic disc surgery can be considered as a first-line surgical option, especially for young women and office workers who are sensitive to scarring and recovery speed.”
Related articles
- [Column] If you want to change your brain, get moving
- Neurosurgeon ordered to pay ₩140 million for failing to anticipate patient movement during spinal procedure
- AI developed for diagnosing lumbar central canal stenosis with abdominal CT scans
- Ankylosing spondylitis, easily mistaken for spinal disease, needs early diagnosis
- Urine acidity identified as predictor of bladder cancer recurrence: study

