One of the cancers that should be suspected when abdominal bloating persists for a long time is ovarian cancer.
For example, Kim, 55, was diagnosed with stage 3 ovarian cancer with the BRCA 1/2 mutation after visiting a hospital with severe bloating in her lower abdomen.
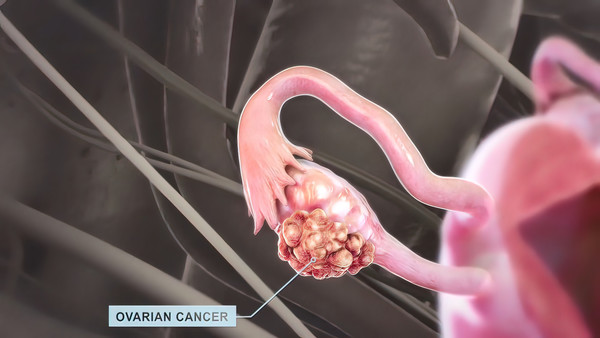
Ovarian cancer originates in the ovaries, fallopian tubes, and peritoneum. It is divided into epithelial ovarian cancer, which accounts for about 90 percent, and non-epithelial ovarian cancer, which accounts for about 10 percent. There are no obvious symptoms in the early stages, and as it progresses, patients may feel bloating due to ascites. If it metastasizes to other organs, especially the lungs, it can cause breathing difficulties due to pleural fluid.
Ovarian cancer marks the lowest survival rate due to lack of early symptoms
Although ovarian cancer has a low prevalence rate of 2.4 percent, it has the lowest survival rate among gynecologic cancers due to its lack of early symptoms.

"The five-year survival rate of ovarian cancer from 2017 to 2021 was 65.7 percent, which is relatively low compared to the average five-year survival rate of cancer patients during the period (72.1 percent). In particular, advanced ovarian cancer has been known to be a difficult and challenging cancer to treat, with a recent five-year survival rate of 45.6 percent," said Professor Kim Jeong-cheol of the Department of Obstetrics and Gynecology at Soon Chun Hyang University Hospital Bucheon.
For epithelial ovarian cancer, the main causes include increased ovulation frequency, genetic predisposition such as BRCA 1/2 mutations, and advanced age.
Pregnancy, breastfeeding, and taking oral contraceptives, which decrease the number of ovulations, have been shown to reduce the risk of developing epithelial ovarian cancer.
Patients with the BRCA 1/2 mutation have a lifetime prevalence of ovarian cancer ranging from 10 to 46 percent. In one study, 45 percent of new cases of ovarian cancer were reported to occur in patients between the ages of 55 and 75. Non-epithelial ovarian cancer, on the other hand, seems to predominate in younger patients.
"Other factors, including menopausal hormone therapy, obesity, polycystic ovary syndrome, and a family history of breast cancer, have been suggested in the literature as contributing factors to ovarian cancer, but they have not yet been identified," Kim said.
Genetic testing and customized treatment could reduce recurrence and death rates
To diagnose ovarian cancer, genetic predisposition is identified through medical and family history, imaging tests (pelvic ultrasound, abdominal CT/MRI, PET-CT, etc.), and tumor marker tests (CA-125, HE4). If ovarian cancer is suspected, a surgical biopsy is performed to confirm the diagnosis.
Treatment for ovarian cancer is a combination of surgery, chemotherapy, immunotherapy, and targeted therapy. Surgery involves a complete laparotomy of the abdominal cavity to remove the female appendages and remove any cancerous lesions in the organ that have metastasized.
Depending on the patient's condition and stage, post-operative chemotherapy and targeted therapy with genetic testing may be performed. If the disease is very advanced, surgery to confirm ovarian cancer may be followed by upfront chemotherapy to shrink the size of the lesion, followed by surgery and chemotherapy, according to Professor Kim.
"In ovarian cancer, personalized treatment with targeted therapies and immunotherapies based on the results of genetic testing has contributed to a decrease in recurrence and mortality rates. In particular, it has recently been reported that drug selection based on BRCA mutations can reduce recurrence and mortality in patients, and even after recurrence, various treatment methods are being devised according to the patient's condition and recurrence characteristics," Kim said.
While prevention of ovarian cancer remains unclear, patients at genetic risk, which accounts for 10 percent of all patients, may be considered for intensive surveillance and risk-reducing surgery, known as bilateral salpingo-oophorectomy.
Continued surveillance, especially if a BRCA 1/2 mutation is identified, may be considered for a short period until age 30-35 before deciding on risk-reducing surgery. Patients with an inherited disorder known as Lynch syndrome also have a reported risk of ovarian cancer of 3-33 percent, so risk-reduction surgery may be an option to lower their risk.
Some reports found that screening for ovarian cancer through transvaginal ultrasound and tumor markers does not significantly improve mortality and survival rates, so frequent screening for ovarian cancer alone is not recommended for the general population who do not carry a genetic mutation, Kim noted.
"While there is still no cure for ovarian cancer, research is helping to personalize treatment for patients. So, it's important to work with your healthcare team to determine the best course of treatment and to be willing to fight the disease."
Related articles
- Extremely rare disease drug Ceprotin clears major hurdle to reimbursement
- [Reporter's Notebook] Genome & Company refused to disclose indications after technology transfer. Why?
- AZ’s next-generation PARP inhibitor Saruparib draws attention at AACR 2024
- Novartis' rare disease drug Ilaris passes health insurance review panel
- Several Korean biotech firms face delisting amid audit failures, financial struggles
- AstraZeneca Korea launches 'Lung Live the Queen' campaign for early detection of lung cancer in women
- Early post-surgery exercise significantly enhances upper limb recovery in breast cancer patients: study
- Ovarian cancer rises among ‘relatively young’ Koreans in their 40s and 50s. Why?
- Which is more accurate in detecting cancer: tissue biopsy or liquid biopsy?

