It has been demonstrated that a single cervical cancer sample can be used to diagnose cancer and analyze the microbiome simultaneously.
In a healthy cervical environment, beneficial bacteria, including Lactobacillus, are predominant and play a protective role against pathogens. On the other hand, an increase in microbial diversity and an increase in specific pathogenic bacteria are associated with a higher risk of HPV infection persistence and progression to cervical lesions, making microbial analysis important in cervical cancer.
Seoul National University Bundang Hospital (SNUBH) said Thursday that a team led by Professor Kim Ki-dong of the Department of Obstetrics and Gynecology and Professor Kim Jun-Mo of the Department of Animal Biotechnology at Chung-Ang University has confirmed it is possible to analyze microorganisms using Liquid-Based Cytology (LBC) specimens used for cervical cancer screening.
Cervical cancer is a cancer of the cervix, the opening to the uterus, and is primarily caused by infection with the HPV (human papillomavirus). Recent studies have shown that various microorganisms present in the cervix closely influence HPV infection and the development of cervical cancer, and interest is growing in analyzing the microbiome of the cervix.
The most basic test for early diagnosis of cervical cancer is the Pap test, which uses a cotton swab or small brush to collect cells from the surface of the cervix and examine them under a microscope. This test has evolved recently, and the liquid cytology test (LBC) has become widely used. Liquid cytology is a method in which the collected cells are soaked in a liquid preservation solution and sent to the laboratory, and it has the advantages of better cell preservation, easier reading, and higher accuracy than conventional cytology.
Cervical microbiology tests, on the other hand, have only been performed for research purposes and use the swab method. This method requires additional testing because microorganisms can be lost during the collection process and must be performed separately from the cytology test. The researchers set out to determine if the liquid cytology test (LBC), which is used to diagnose cervical cancer, could also be used to analyze microorganisms.
The team analyzed the microbial communities of 30 female participants by comparing LBC and swab samples. The results showed that LBC samples yielded similar levels of microbiome data to swab samples, with similar proportions of key microbial communities, such as Lactobacillus and Gardnerella.
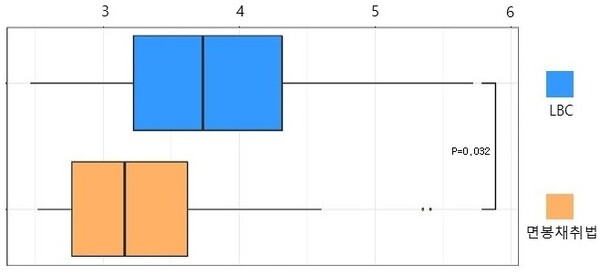
Notably, the Alpha Diversity Index, which measures the diversity of microorganisms in a sample (the higher the number, the more diverse), showed that LBC samples had higher microbial diversity than swab samples. This supports the possibility that LBC samples are more favorable for microbial analysis.
The study is significant because it confirms that LBC samples, which are collected annually from millions of women worldwide, are a valuable resource for cervical microbiome analysis. This opens the door to more precise and multifaceted analyses of cervical cancer screening using already collected samples.
“The ability to obtain two important pieces of information from a single specimen is a new opportunity for cervical cancer diagnosis,” Professor Kim Ki-dong said. “This study will help us understand the relationship between cellular abnormalities and changes in the microbiome, which could lead to the development of new biomarkers for early detection of cervical cancer.”
Related articles
- Cancer immunotherapy that reflects Asian patients' characteristics will arrive soon
- Noul secures FDA Class 1 approval for miLab diagnostic solutions
- Opposition lawmaker questions President Yoon's unfulfilled HPV vaccine promise as cancer cases rise
- National screening policy is key to eradicating cervical cancer: NCC study

