A joint research team at Yonsei University College of Medicine and Severance Hospital has uncovered how specific regulatory T cells drive the anti-inflammatory effects of allergen-specific immunotherapy in patients with atopic dermatitis, shedding light on the cellular mechanisms behind this common allergy treatment.
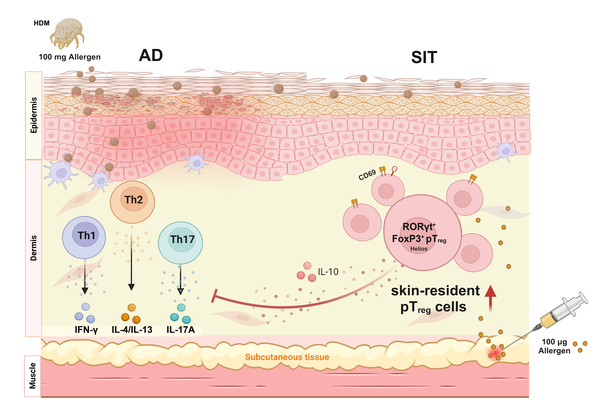
Atopic dermatitis, a chronic inflammatory skin condition, is often triggered by allergens such as house dust mites penetrating a damaged skin barrier. This intrusion activates pathogenic T cells -- such as Th1, Th2, and Th17 subsets -- which release inflammatory cytokines and perpetuate chronic immune responses.
Subcutaneous immunotherapy (SIT), commonly used to treat allergic conditions like atopic dermatitis, works by gradually exposing patients to allergens in order to train the immune system to reduce its hypersensitive reactions. The repeated administration of allergens beneath the skin is designed to activate skin-resident regulatory T cells (Tregs), which suppress excessive immune responses.
As a result, the research team, led by Professors Park Chang-ook of the Department of Dermatology, Park Jung-won of the Department of Internal Medicine, Sohn Myung-hyun of the Department of Pediatrics at Severance Hospital, and KeLun Zhang and Lee Kwang-hoon of the Department of Dermatology and Cutaneous Biology Research Institute, and Kwon Ho-keun of the Department of Microbiology and Immunology at Yonsei University College of Medicine, sought to identify which Tregs specifically contribute to the immunotherapy’s success.
The team examined peripheral blood mononuclear cells (PBMCs) from both human patients with atopic dermatitis who responded to SIT and from mouse models.
By analyzing the transcriptional profiles of Tregs, they identified a subset that expresses the transcription factor RORγt, which is known to regulate T cell differentiation and function.
These RORγt-expressing regulatory T cells were found in higher levels in both blood samples and skin tissues of patients following successful SIT. In mouse models, these cells also accumulated in the skin and exhibited potent anti-inflammatory effects by suppressing pathogenic T cell activity.
Further functional studies demonstrated that RORγt-positive Tregs are instrumental in mediating the therapeutic effect of SIT by downregulating immune responses associated with chronic inflammation in atopic dermatitis.
“Understanding the diversity and function of immune cells in the skin is the starting point for building a human skin immune atlas and advancing cell-based immunotherapies,” Professor Park Chang-ook said. “By elucidating the mechanism of subcutaneous allergen-specific immunotherapy, our findings are expected to enhance the precision and effectiveness of immune-based treatments for atopic dermatitis and other inflammatory skin diseases.”
The results were published in the Science Translational Medicine.
Related articles
- Severance team develops 3D organoid to predict pancreatic cancer drug response
- Severance Health Check-Up named Korea’s top consumer-recommended premium screening center
- Immune cells supercharge aspirin delivery, boosting transfer up to 30-fold: Yonsei study
- [Interview] Cracking cancer’s cold cases: the startup that may have found immunotherapy’s blind spot
- Severance Hospital tops KS-WEI list for 19 straight years
- Psychiatrist calls for new mindset to overcome psychological burden of atopic dermatitis
- CMS Lab unveils next-gen Barrierderm MD Cream for skin restoration in AD patients

