
Fourteen years and six months vs. one year.
According to the Ministry of Food and Drug Safety, it takes at least 14-and-a-half years to develop a new drug.
In detail, five years are needed to select candidate substances, one-and-a-half years for preclinical trials, six years for clinical trials, and two years for reviewing permits and giving approvals.
However, it took Moderna only 11.2 months to develop its Covid-19 vaccine. The company began development on Jan. 13, 2020, and received final approval on Dec. 19. Pfizer even spent less time, starting development on Jan. 13 and getting the nod on Dec. 2, 2020 (10.8 months).
The drastic difference in the development period of new drugs that require the confirmation of efficacy and safety was partly due to the government’s financial and systemic support amid the special pandemic. However, no less important than that was technological development. Decentralized Clinical Trials (DCT) also played a key role in developing vaccines by making clinical trials possible where movements were restricted for fear of infections.
DCT proved efficacy and safety a decade ago
In developing its Covid-19 vaccine (mRNA-1273), Moderna introduced Medidata’s Reve platform, a cloud-based solution, to conduct clinical trials more efficiently and swiftly. The company could recruit 30,000 clinical trial subjects quickly through the Rave platform and the integrated use of clinical solutions, such as electronic data capture (EDC), electronic clinical outcome assessment (eCOA), and central statistical analytics (CSA).
Other Covid-19 vaccine developers, such as Pfizer, BioNTech, and AstraZeneca, also conducted clinical trials using the DCT method, like the Rave platform.
DCT drew attention because of the Covid-19 vaccine development. However, its initial use traces back to 2011 when Pfizer conducted a phase 4 trial for Tolterodine. The company conducted the trial to treat oversensitive bladder by recruiting subjects and collecting data on the web without forcing subjects to visit medical institutions.
The study drew attention because one of its major objectives was to know whether virtual clinical trials like DCT would be feasible. For that purpose, researchers included comparing the digitalized clinical trial with the current phase 4 clinical trial in the assessment.
In the Tolterodine study, regional doctors conducted medical checkups of trial subjects and used an online identification confirmation method by a third party called IDology, GA, USA, to identify participants. After multiple-choice testing, the preliminary consent process was conducted in an interactive web-based method, and drugs were directly delivered to participants. As a result, the web-based DCT method showed equal efficacy and safety to traditional clinical trials.
Besides, BioTissue, a U.S. bio company, applied DCT to its phase 3 pivotal clinical trial to treat severe diabetic foot ulcer amid the lockdown to prevent the spread of Covid-19 in March 2020.
There are more cases of large-scale research using DCT. A case in point is the ADAPTABLE (Aspirin Dosing: A Patient-centric Trial Assessing Benefits and Long-term Effectiveness) study, one of the largest DCT studies in which about 15,000 subjects participated.
The U.S. Patient-Centered Outcomes Research Institute (PCORI) conducted the study to evaluate the optimal dose of aspirin for patients with heart disease. The study was conducted on heart disease patients with an average age of 67 using a 100 percent DCT method without hospital visits. Researchers maintained a high participation rate of 95 percent until the final process by increasing the understanding of subjects through eConsent, Medidata’s clinical trial platform.
“From Pfizer’s Tolterodine to Moderna’s Covid-19 vaccine, the decade-long period proved that DCT did not remain at a conceptual level but is a practical method that supplements or improves existing clinical trials,” KoreaBio said. “DCT has its limitations, but its advantages are certain to improve new drug development process.”
The association of bio companies said, “In Korea, too, various related sectors should have interests in making the most of DCT amid the positive participation of interested parties, the government’s active forward-looking deregulation, and vigorous investment in startups developing clinical solutions.”
Domestic industry moves to introduce DCT
There are also moves in the domestic industry to change clinical trial culture by introducing DCT.
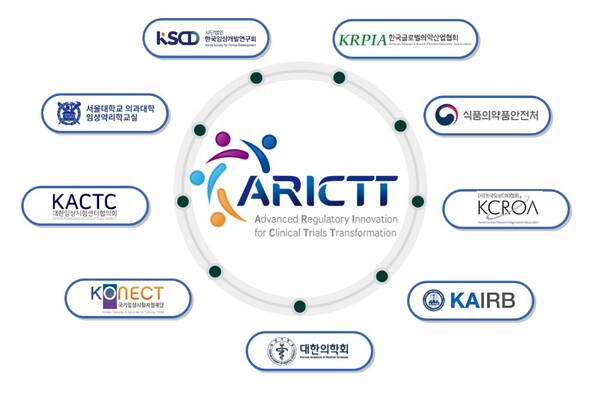
First, the Ministry of Food and Drug Safety has recently established a platform called ARICTT (Advanced Regulatory Innovation for Clinical Trial Transformation), discussing DCT-related issues.
At an ARICTT symposium in December, Professor Huh Ki-young of the Department of Pharmacology at Seoul National University Hospital presented an example of conducting clinical trials in a 100 percent DCT way to work out DCT guidelines.
The DCT case, planned as a pilot program, was a mock study where researchers gathered patients’ data using telemedicine, videos, phones, and websites without forcing subjects to visit medical institutions even once.
The study was conducted not to discover lactobacillus's effects on constipation but to know what problems can occur when they use DCT in clinical trial procedures. Under the current law, specialized medicines have delivery problems, so they use health-functional foods that anyone can buy in markets.
The researchers divided constipation patients into lactobacillus + vitamin C group and vitamin C only group. Participants then received health-functional foods after being randomly allocated into patient groups through tele-screening. Afterward, they collected stool samples at home and sent them back to the research institutions, and researchers collected patients' data using apps.
Researchers also received reviews from subjects. “It was good because I had only to participate through an app without visiting the institutes,” one participant said. “I felt the barrier to participating in clinical trials was lowered.”
Asked to point out problems for improvement, the subject said, “When the clinical trial schedule was confusing, I had to check the consent form, but it was uncomfortable because I couldn't see it at once. I sometimes forgot to take the drug on time when I went out. There were days when I tried to care for myself but couldn’t.”
Professor Huh said, “The most difficult part (in performing DCT) was to ensure the compliance of the test subjects. In addition, due to its non-face-to-face characteristics, more detailed explanation and efficient management procedures are required.”
Professor Yu Kyoung-sang of the same department, who co-led the study, said, “The advantages and disadvantages of DCT earned in the study will be reflected in the domestic DCT guidelines. I hope these factors will be considered to help the successful conduct of DCT in earnest in the future.”
Related articles
- [Special] 'Be it US, Europe, or China, DCT is global trend in clinical trials'
- [Special] Decentralized clinical trial is not an option but a must
- [Special] ‘Regulation’ blocks DCT introduction in Korea. So how to unravel tangled threads?
- [KIMES 2023] ‘Medical devices should be similar for FDA 510(k) but differentiated for sales’
- Decentralized clinical trial emerges as irresistible trend. What about Korea?
- Clinical trials are shifting towards DCT but hybrid approach more likely: IQVIA execs
- Regulator ‘half-positive’ to digital healthcare firms' request to introduce DCTs
- JNP MEDI's pioneering role in DCT unveils enormous potential
- Korea's delay in decentralized clinical trials sparks global exclusion concerns: experts

