A recent study has argued that the earlier patients use BMS’ Abecma, the first CAR-T (chimeric antigen receptor-T cell) treatment of multiple myeloma, the stronger its effects can become, drawing the academic community’s attention.
Tuesday (local time), the American Society of Hematology introduced the results of the KarMMa-2 study, the phase 2 clinical trial of Abecma, released at ASH 2022, in its newsletter.
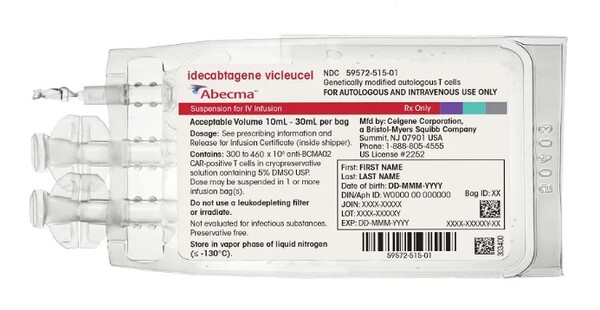
Abecma, a CAR-T immunotherapy targeting B cell maturation antigen (BCMA), is the first treatment approved for curing multiple myeloma.
In the United States, it won approval for recurrent, refractory patients who have received four or more times of treatments with immunomodulators, proteasome inhibitors, and anti-CD38 monoclonal antibodies in March of last year and has since been used by them.
However, according to Dr. Krina Patel of the University of Texas MD Anderson Cancer Center, who released the KarMMa-2 study results, patients who recurred early after primary treatment showed a worse prognosis.
Dr. Patel said that if it recurs within 12 months of the primary treatment, the overall survival (OS) is only about 26 months, which shows a wide gap with 91 months in patients who experience recurrence later.
“To improve the results in these vulnerable patients, a therapy with a new mechanism of action is urgently needed,” she said.
The KarMMa-2 study was the phase 2 clinical trial to evaluate the safety and efficacy of Abecma in patients who experienced early recurrence after primary treatment or showed improper response after transplantation. It was composed of three cohort groups, and the data released this time resulted from cohort 2a.
Patients included in cohort 2a recurred within 18 months after receiving induction therapy, transplantation, and a lenalidomide-based maintenance regime as primary treatment.
“Researchers injected ide-cel in 37 patients,” the ASH said. “At the start of the study, 5.4 percent of patients were in phase 3 according to the revised international disease recording system, 32.4 percent were a high-risk group in cytogenetics, and 8.1 percent had diseases other than bone marrow problems.”
This notwithstanding, 83.8 percent of patients showed responses to treatment, it said, adding that the median value until responses was about one month, which is common in CAR-T treatment.
Besides, although the median duration of response (mDoR) in total patients was 15.7 months, in the case of patients who showed complete response (CR), the comparable figure was 23.5 months, indicating that those who showed deeper responses also experienced long periods of responses.
Notably, 45.9 percent of patients showed CR at the median value of the follow-up observation period of 21.5 months, and only 22 percent showed CR during the primary treatment period.
The median progression-free survival (mPFS) was 11.4 months, median overall survival (mOS) has yet to reach the median value, and 84.7 percent of patients were alive at the 24th month.
All patients administered with Abecma showed side effects of three to four grades, but most of them were related to hematology, such as neutropenia (94.6 percent), anemia (45.9 percent), and thrombopenia (37.8 percent).
Of the total participants, 83.8 percent experienced cytokine release syndrome (CRS) of first to three degrees, and 21.6 percent, neurological toxicity of first to second degrees.
“Ide-cel showed frequent and deep responses in clinically high-risk myeloma patients who experienced early recurrence within 18 months of the frontline treatments, including transplantation,” Dr. Patel said. “These high response rates were encouraging among patients hard to treat.”
She said, “If we use ide-cel far earlier than the approved fifth treatment, it will make far bigger differences in more patients.”

